Exocrine Pancreatic Insufficiency (EPI)
Your gastrointestinal tract is made up of several vital organs responsible for executing critical tasks, such as absorbing and processing the vitamins and minerals in the foods you consume, aiding in the digestion process, and eliminating waste materials.
If asked to name organs in this important body system, you could probably name the stomach and intestines. A crucial but sometimes overlooked component is the pancreas. This organ performs several vital roles and, when ailing, can interrupt several key processes.
When the pancreas malfunctions, you could be susceptible to any number of pancreas-related problems. One specific condition is called exocrine pancreatic insufficiency.
Exocrine Pancreatic Insufficiency Overview
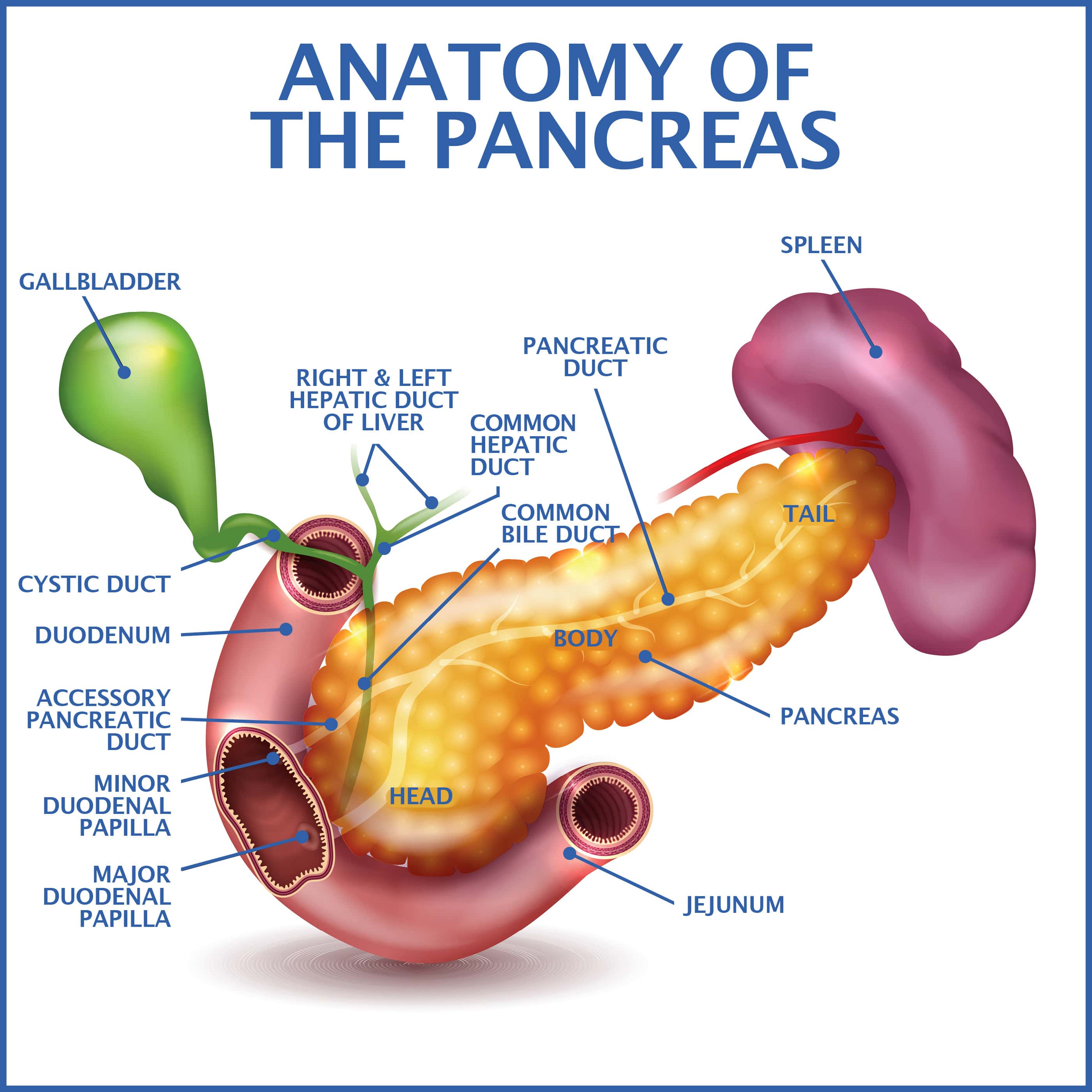
The pancreas carries out many key functions. This tiny gland is situated near the stomach, liver, and small intestine and regulates the body’s glucose (sugar) concentrations.
The pancreas also produces critical chemicals known as enzymes. Exocrine pancreatic enzymes are important to the body’s capacity to digest food properly. If you are diagnosed with exocrine pancreatic insufficiency (sometimes abbreviated as EPI), the pancreas fails to produce enough of these substances.
Causes
The primary underlying causes of exocrine pancreatic insufficiency are disease and damage to the pancreas.
Risk Factors
Specific risk factors can increase your chances of contracting the condition, such as:
- Inflammation – Systemic inflammation occurring in and around the pancreas can bring forth or aggravate the issue. Typically, such events are caused by chronic, heavy alcohol usage or some type of pancreatic disease.
- Digestive Tract Surgery – If you underwent surgery to remove or repair certain parts of the gastrointestinal system, your risk is higher.
- Systemic Illnesses – A variety of gastrointestinal ailments can ultimately impact pancreatic function and raise the chance for exocrine pancreatic insufficiency, including:
- Celiac disease, which is intolerance for gluten.
- Inflammatory bowel diseases like Crohn’s and ulcerative colitis can irritate the lining of the digestive tract, interfere with the body’s ability to process nutrients, and ultimately result in EPI.
- Autoimmune disorders like lupus, autoimmune pancreatitis, and cystic fibrosis can inhibit proper pancreatic operation, block enzyme production, and eventually precipitate EPI.
The most significant offending illness is diabetes. Diabetes is your pancreas’s inability to appropriately regulate blood sugar levels due to diminished quantities of insulin.
Symptoms
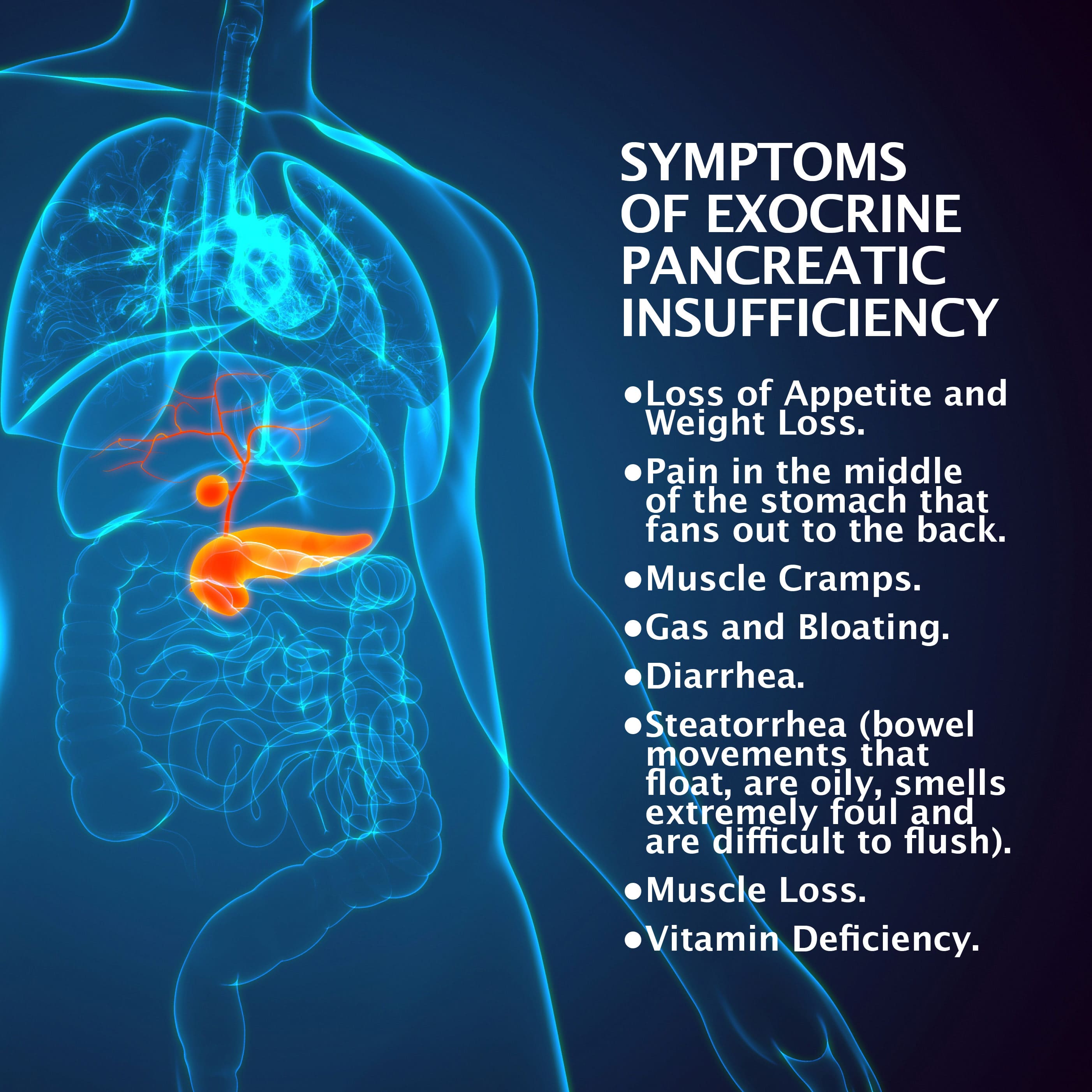
During exocrine pancreatic insufficiency’s initial stages, you may not experience any physical symptoms. But as pancreatic deterioration worsens, symptoms ultimately emerge and often include:
- Abdominal pain.
- Diarrhea.
- Unintentional weight loss.
- Bloating.
- Feeling of fullness.
- Increased gas.
- Malodorous bowel movements.
In more advanced cases, your body often experiences difficulties absorbing nutrients. This can result in a host of potentially serious outcomes.
Diagnosis
Unfortunately, EPI symptoms mimic those seen in many other illnesses. A diagnosis could take some time and need several diagnostic tests, such as:
- Blood Tests – Enables your physician to determine if your body is absorbing enough vitamins and minerals. Blood tests will help conclude if your pancreas is producing enough enzymes. Additionally, blood tests can help identify potential underlying issues, most notably celiac disease.
- Stool Examinations – The consistency, content, and quality of your stools are often a valuable diagnostic tool. Specific stool tests employed to diagnose EPI include:
- The Three-Day Fecal Test – If asked to undergo this procedure, you will be required to collect small samples of your bowel movements over three days, place them inside separate containers, and label them in chronological order. The contents are examined for fat accumulation over this three-day duration.
- Fecal Elastase-1- You collect specimens of your stool, store them in a container, and return it to your doctor. Then a laboratory will study the contents for critical digestive enzymes. If these chemicals are not detected, you may have exocrine pancreatic insufficiency.
- Internal Imaging Scans – Your doctor might order various internal imaging scans to determine if your pancreas is inflamed or damaged. These include endoscopic ultrasound, CT (computed tomography), and MRI (magnetic resonance imaging) scans.
Treatment Options
Fortunately, EPI is controllable through various treatment efforts such as:
- Enzyme Replacement Therapy – This treatment, known as PERT, or Pancreatic Enzyme Replacement Therapy, is designed to replace the essential chemicals the pancreas cannot synthesize. These substances help your digestive system process food and absorb vitamins and minerals with greater speed and efficacy. The following medications are sourced from the pancreas glands of pigs and only available with a prescription:
- Creon.
- Pancreaze.
- Pertzye.
- Ultresa.
- Viokace.
- Zenpep.
- Medications – Your doctor might place you on a therapeutic regimen of prescription or over-the-counter drugs to control gas, discomfort, and diarrhea.
- Proper Nutrition – The most crucial aspect of exocrine pancreatic insufficiency therapy is ensuring you remain adequately nourished. Nutritionists and medical professionals stress that circumventing EPI necessitates an increased intake of vital nutrients, such as carbohydrates, proteins, and fats. Carbohydrates are abundant in foods like pasta and grain products. Fats are found in edible items such as dairy products and nuts. Foods like poultry, fish, and meat are rife with energy-building proteins.
- Dietary Augmentation – Dietary augmentation with vitamin and mineral supplements also proves critical. EPI often causes a rapid depletion of essential nutrients. A healthy, balanced diet typically is not enough. Dietary supplementation is vital to maintaining normal systemic concentrations of such products.
Prognosis
Presently, exocrine pancreatic insufficiency has no known cure. But the condition can be controlled by addressing specific underlying causes and adhering to a proper diet. If so, you can live a normal, productive, and potentially lengthy life.
Prevention
Certain types of EPI cannot be prevented. EPI caused by inherited or genetic conditions is impossible to stop.
Other instances may be preventable if you follow suggestions like exercising routinely, maintaining a healthy weight, limiting alcohol consumption, curtailing or quitting smoking, limiting fat consumption, and avoiding crash diets.
Additionally, you should get routine medical care. During these checkups, your doctor can identify any potential precipitating conditions and properly address them.
Contact Us
Even in a mild form, exocrine pancreatic insufficiency can be painful and debilitating. More severe cases can be disabling and carry the potential to elicit serious health issues. Reaching out to a professional is a must.
Our practice began more than 15 years ago and has emerged as one of the leading gastroenterology practices in central Florida. We perform a host of diagnostic procedures using state-of-the-art equipment in a friendly, comfortable, and inviting atmosphere where patient care is always a top priority. Contact us today!