
Common Gastrointestinal (GI) Problems in Men
Anyone is susceptible to gastrointestinal problems. Some GI disorders affect a higher percentage of men than women. Some need minimal treatment, while others could be life-threatening. Here are several of these gastrointestinal conditions and how they can be treated.
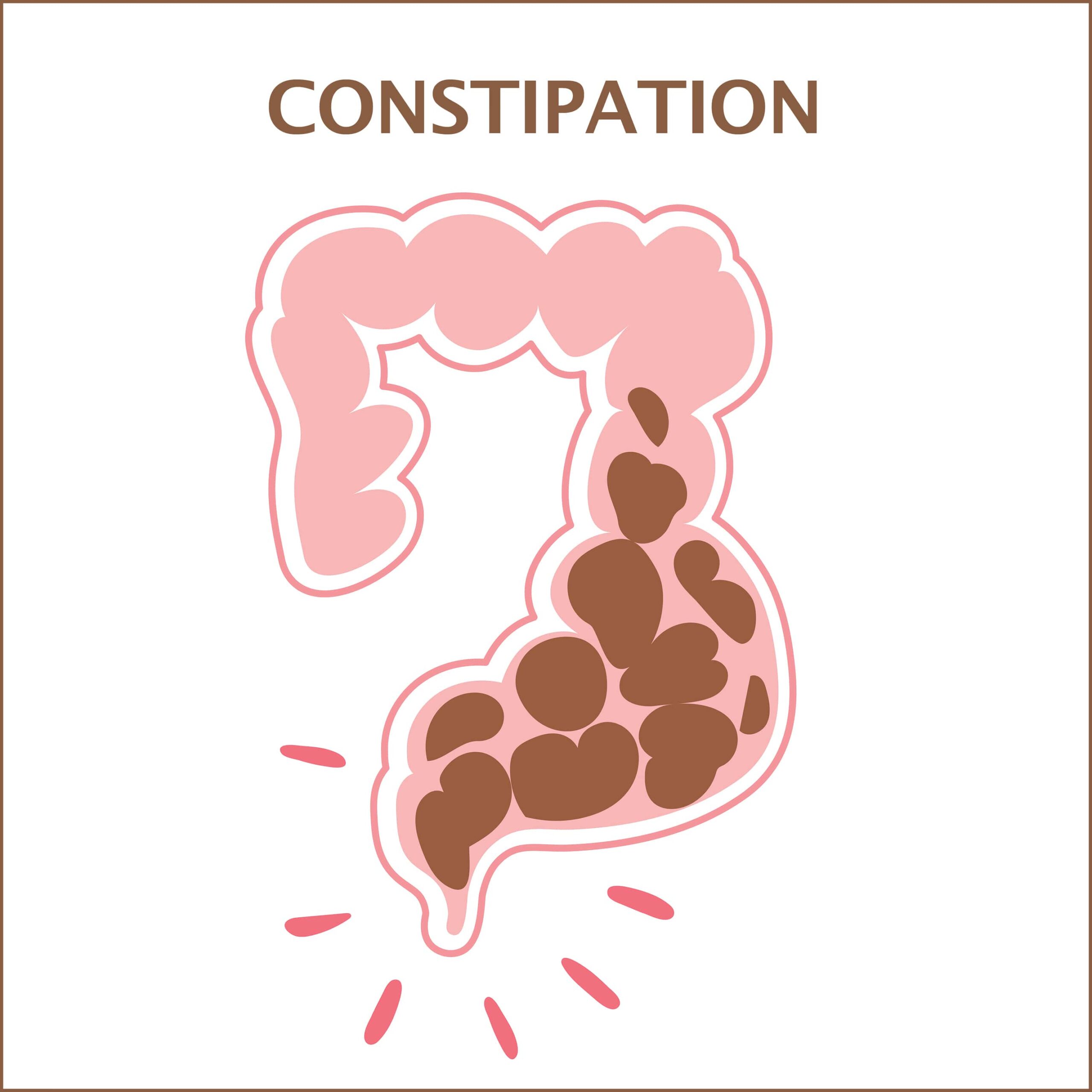
1. Constipation
Chronic (long-term) constipation is a disorder that is especially common in older men. If you have constipation, your bowel movements become hard and dry. This makes them infrequent and difficult or painful to pass.
Nutrients are absorbed from food as it travels through the digestive tract. The remaining waste is transferred from the small intestine to the large intestine (colon). The colon then absorbs water from this substance, turning it into a bowel movement. The more slowly this waste passes through the intestine, the more water will be absorbed, resulting in a dryer, harder stool.
Many things can cause constipation, including:
- A low-fiber diet.
- Ignoring the urge to go to the bathroom.
- Dehydration.
- Antidepressants.
- Non-steroidal anti-inflammatory drugs (NSAIDs).
- Neurologic disorders.
- Endocrine problems.
Another cause of constipation can be the overuse of laxatives because they can be habit-forming. Your body becomes dependent on them, increasing your chances of constipation if you stop them.
You’ll know that you’re constipated if:
- You have hard, painful stools.
- You strain to go to the bathroom.
- You feel as though you haven’t completely emptied your rectum.
Typically, you can treat constipation yourself by:
- Eating high-fiber foods.
- Staying active.
- Drinking plenty of water.
- Going to the toilet when you first feel the urge.
- Avoiding alcohol and caffeine.
If these home treatments aren’t effective, your doctor may prescribe medication. Surgery, which is rarely used to treat constipation, may be necessary if your intestine has a defect such as a stricture, blockage, or anal tear.
2. Gastroesophageal Acid Reflux Disease (GERD)
Gastroesophageal acid reflux is a condition in which gastric juices back up into the esophagus (food pipe), causing a burning sensation in your chest.
The condition develops when the lower esophageal sphincter (LES) at the junction of the stomach and the esophagus opens and closes incorrectly. Usually, the LES opens so that food can enter your stomach and then closes, so that stomach acid doesn’t leak back into your esophagus. If you have a weak LES, it can’t prevent acid from backwashing and causing indigestion or heartburn. Men are more likely than women to have a weak LES, making them more prone to damage from stomach acid.
The main symptom of GERD is heartburn, which feels like a burning sensation from your breastbone to your neck. Other symptoms may include:
- Difficulty swallowing.
- Regurgitation.
- Tight throat.
- Bad breath.
- Feeling as though there’s a lump in your throat.
GERD can be aggravated by:
- Smoking.
- Eating large meals.
- Eating meals late at night.
- Drinking alcohol or coffee.
- Taking medications such as aspirin, ibuprofen, or naproxen. These types of medicine could aggravate the condition or, in rare cases, cause stomach or intestinal bleeding.
GERD is sometimes confused with a heart attack. Even though it’s called heartburn, it’s unrelated to your heart. A heart attack causes shortness of breath, dizziness, sweating, and pain in your arms and jaw.
Long-term GERD can trigger significant health issues such as:
- Strictures.
- Inflammation of the esophagus.
- Barrett’s syndrome (a condition in which the cells lining your esophagus become abnormal from prolonged exposure to stomach acid).
GERD can typically be managed with antacids that you can buy at a drugstore. If symptoms are resistant, a surgery that reinforces the lower esophageal sphincter can be performed.

3. Diarrhea
Men are more susceptible to diarrhea than women because stools pass through their system faster. This produces watery, loose bowel movements because they don’t have enough time to harden. Diarrhea is a common problem that usually only lasts a few days.
Diarrhea can be caused by:
- Bacteria from contaminated food or water.
- Viruses.
- Parasites.
- Food intolerances.
- Medications.
- Eating irritants such as spicy foods.
Sometimes there’s no clear cause of diarrhea, and it resolves on its own.
The symptoms of diarrhea include:
- Abdominal cramps.
- Bloating.
- An urgent need to defecate.
- Nausea.
These symptoms are uncomfortable but not dangerous, and you can usually treat them yourself. Since you lose a good deal of liquid each time you defecate, you’ll need to drink plenty of water, broths, or fruit juices. A sports drink can help replace electrolytes. Additionally, eat mild foods, including:
- Toast.
- Yogurt.
- Crackers.
- Scrambled eggs.
- Oatmeal.
- Bananas.
Some foods irritate the digestive tract and can trigger or worsen diarrhea. These include:
- Fried foods.
- Spicy foods.
- Coffee.
- Alcohol.
- Fatty meats.
- Dairy products.
Sometimes self-care isn’t enough to manage your condition. You’ll need to see a doctor if you have:
- Intense abdominal pain.
- Black or bloody stools.
- A fever of 102 degrees or more.
- Diarrhea that lasts more than two days without improvement.
If you have these symptoms, your doctor will perform tests to determine if an underlying health issue is causing your condition. These procedures can include:
- Blood test.
- Stool test.
- Colonoscopy (for examining your entire colon).
- Upper endoscopy (for examining your stomach and upper small intestine).
4. Colon Cancer
According to the American Cancer Society, men have a higher risk of developing colon cancer than women, and it’s one of the deadliest cancers. If caught early, it’s highly treatable. It’s also one of the most preventable of all cancers.
This is because it starts as a polyp (a small growth on the intestinal wall) that takes about ten years to turn cancerous. Because of this, slow growth can be detected in its early stages and stopped in its tracks.
Polyps typically have no symptoms, so early detection of colon cancer is done with a stool blood test. This test identifies hidden (occult) blood in the stool. A colonoscopy is performed to determine if polyps are present when a stool test is positive. Colonoscopy is considered the gold standard of colon cancer treatments because it can detect and remove polyps in a single procedure. If polyps are found, they can be removed when they’re precancerous before any damage has been done.
You should start getting colonoscopies at age 45 and every ten years after that. If you have a history of colon cancer, previous family history of colon cancer, previous polyp removal, or inflammatory bowel diseases, your doctor may recommend getting screened more often.
You can lower your risk of colon cancer by:
- Staying physically active.
- Eating less processed and red meats.
- Eliminating alcohol.
- Quitting smoking.
- Eating whole grains, fruits, and vegetables.
5. Ulcerative Colitis
Ulcerative colitis (UC) is a chronic inflammatory bowel disease (IBD) that causes irritation and ulcers in your colon’s lining. More men in their 50s and 60s are afflicted with IBD than women of the same age.
Your body’s immune system normally defends you against intruders such as viruses and bacteria. When you have ulcerative colitis, your immune system mistakes its own healthy tissue as an invader and attacks it.
There are three types of ulcerative colitis:
- Ulcerative Proctitis – This is the mildest type of UC because the inflammation is restricted to the anus.
- Left-Side Colitis – This type of UC causes pain on the left side of your stomach.
- Pancolitis – Pancolitis impacts the entire colon.
Ulcerative colitis symptoms can include:
- Abdominal cramping and pain.
- Rectal pain.
- Rectal bleeding.
- Weight loss.
- Urgent need to have a bowel movement.
- Diarrhea containing pus or blood.
- Fatigue.
Typically, UC flare-ups come and go, and the periods in between are called remission. Remission may be months or even years.
Although ulcerative colitis is incurable, it can be managed with medications, including:
- Anti-inflammatory medications.
- Immune system suppressors.
- Biologics.
- Anti-diarrheal medicines.
- Pain relievers.
- Antispasmodics.
You can also play a role in managing your UC by:
- Drinking plenty of water.
- Limiting dairy products.
- Avoiding alcohol, caffeine, and carbonated drinks.
- Eating five or six small meals a day instead of three large ones.
- Exercising.
Contact Us
Although men and women can both suffer from the above issues, men are more prone to them. If you have any of these conditions or suspect you do, our team is committed to finding answers about what’s causing your discomfort and putting you on an effective course of treatment.
Our practice began more than 15 years ago and has emerged as one of the leading gastroenterology practices in central Florida. We perform various diagnostic procedures using state-of-the-art equipment in a friendly, comfortable, and inviting atmosphere where patient care is always a top priority. Contact us today!