Celiac Disease: Signs, Symptoms, and How to Manage It
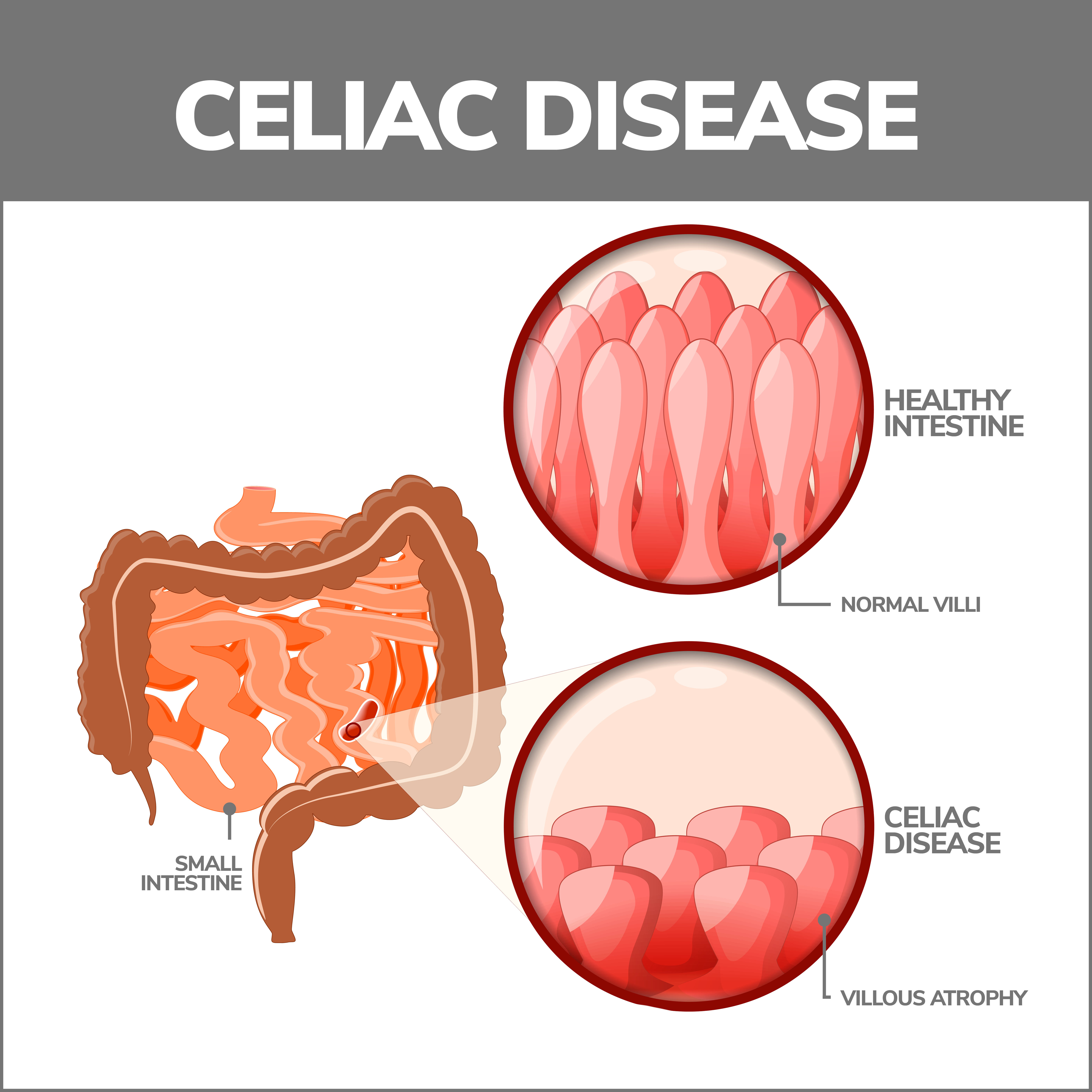
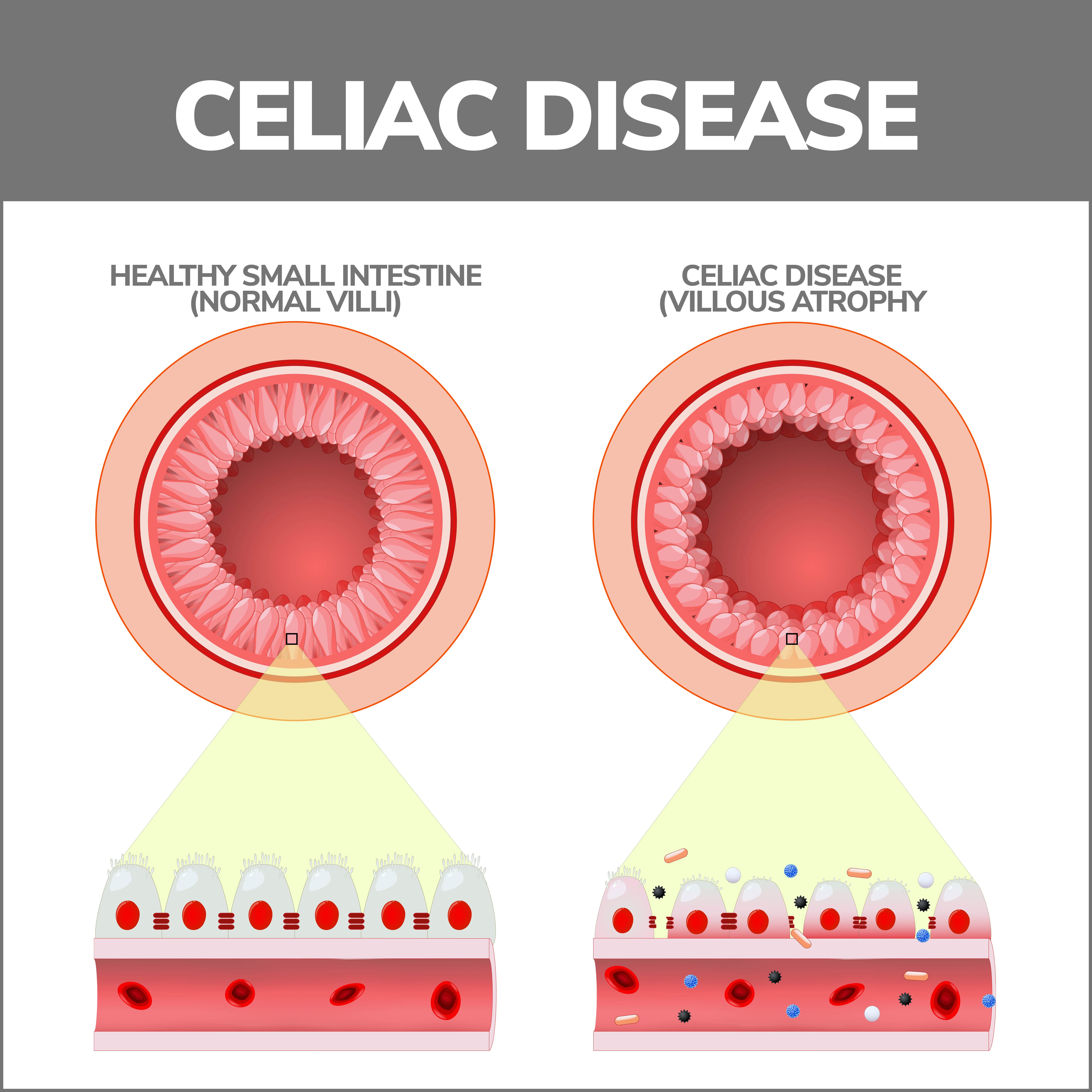
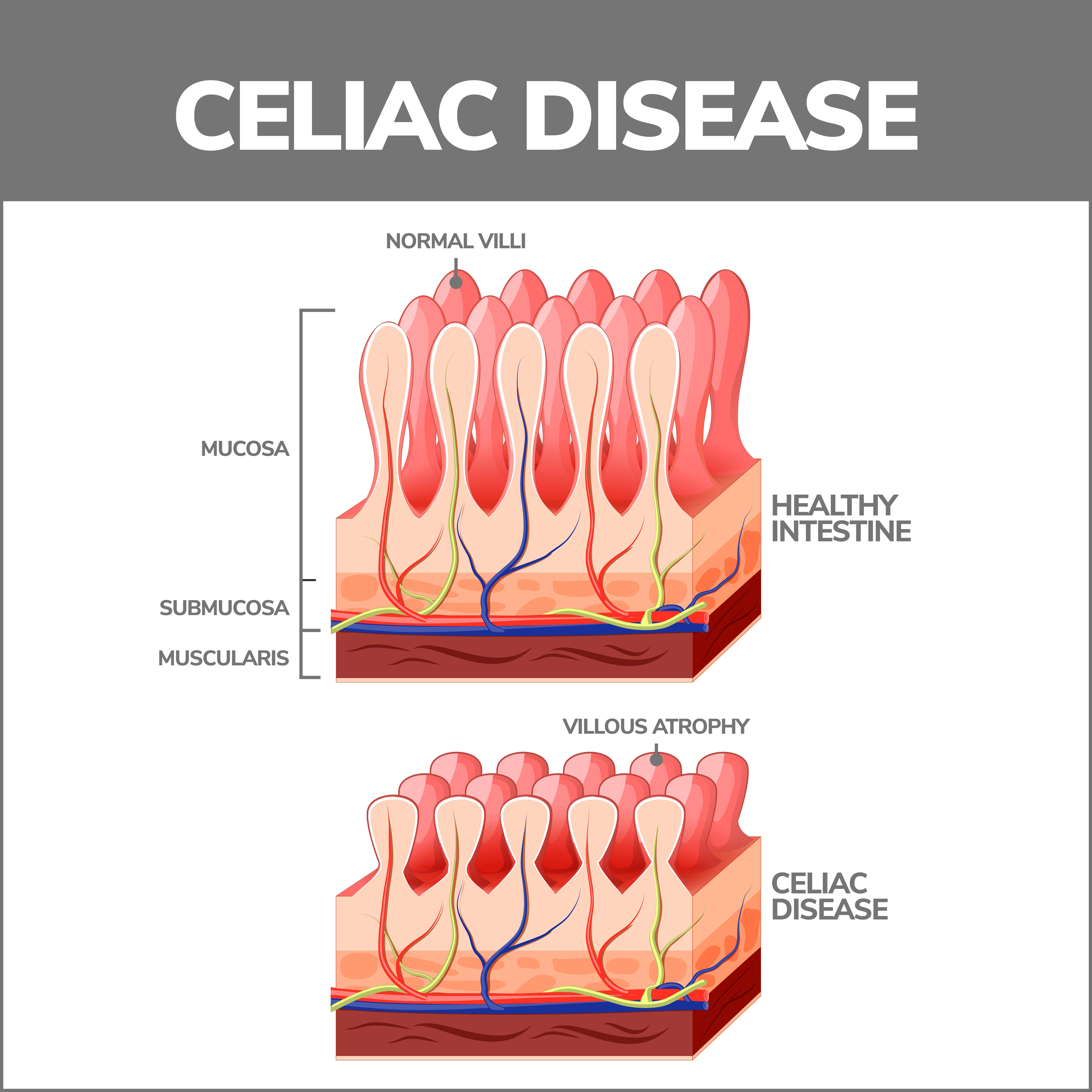
Celiac disease (also called celiac sprue or gluten-sensitive enteropathy) is a serious autoimmune response that damages the small intestine if you eat gluten. Gluten is a protein that’s found in rye, wheat, and barley. It can also be in non-food items such as lip balm, vitamins, toothpaste, and hair and skincare products. If you have celiac disease and eat anything containing gluten, your immune system mounts a defense that damages your small intestine. Over time, these attacks damage the villi, tiny fingerlike structures that line the small intestine and absorb nutrients from the food you eat. Untreated, celiac disease can make you very sick or put you at risk for an early death.
How Do You Get Celiac Disease?
Celiac disease can be inherited. This means it’s genetic – passed from parents to children. Not everyone whose parents have it gets celiac disease, and not everyone who develops it has these genes. While more analysis is needed, some studies have shown that it may also be triggered by:
- Extreme stress.
- Surgery.
- Pregnancy.
- Childbirth.
- Infection.
- Physical injury.
Is Irritable Bowel Syndrome (IBS) the Same as Celiac Disease?
No. Celiac disease is an autoimmune illness that occurs in the small intestine and causes serious damage. IBS is a problem with how the bowels work.
Is There a Cure for Celiac Disease?
There is no cure for celiac disease. It may be manageable if you follow a rigorous, gluten-free diet.
How Do I Know if I Have Celiac Disease?
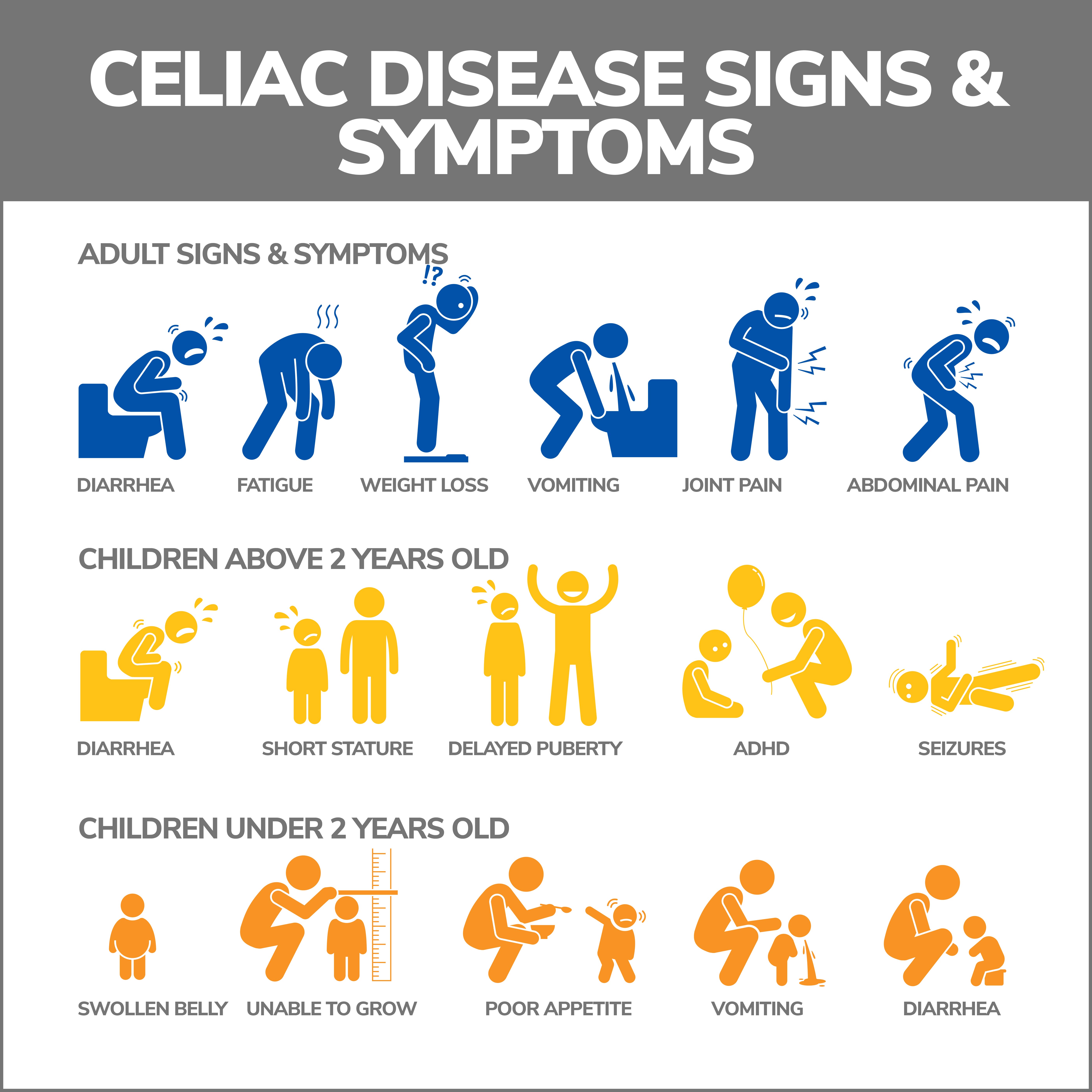
After eating gluten, adults may have signs and symptoms including:
- Abdominal pain.
- Bloating.
- Anemia.
- Constipation.
- Diarrhea.
- An itchy, blistery rash called dermatitis herpetiformis can affect the elbows, knees, buttocks, lower back, or scalp.
- Mouth ulcers.
- Gas.
- Pale, smelly bowel movements.
- Weight loss.
- Fatigue or headaches.
When your villi are severely damaged, the small intestine’s inability to absorb nutrients from food can lead to serious, long-term complications, including:
- Loss of bone density (osteoporosis).
- Weak bones (osteopenia).
- Malnourishment.
- Compromised immunity.
- Neurological damage.
- Permanently damaged tooth enamel.
- Miscarriage and infertility.
- Additional food sensitivities, such as lactose intolerance.
- Pancreatic disease.
- Scarring and ulceration of the small intestine.
- Liver disease.
- Collagenous sprue – This rare disease causes permanent collagen deposits to fill your small intestine’s lining and prevent nutrient absorption.
- Intestinal lymphoma and small bowel cancer.
Children with celiac disease are more prone to intestinal issues, including:
- Constipation.
- Diarrhea.
- Pale, smelly bowel movements.
- Bloating.
- Upset stomach/vomiting.
- Weight loss.
If celiac disease continually prevents a child’s body from absorbing nutrients, they may develop issues including:
- Damaged tooth enamel.
- Delayed puberty.
- Failure to thrive (in infants).
- Irritability or mood changes.
- Slow growth and short stature.
How is Celiac Disease Diagnosed?
Celiac disease can be hard to diagnose because its symptoms often mimic those of other diseases, including:
- Ulcerative colitis.
- Infected colon (diverticulosis).
- Irritable bowel syndrome.
- Crohn’s disease.
- Bacterial overgrowth in the small intestine.
- Iron-deficient anemia caused by menstrual blood loss.
- Chronic fatigue syndrome.
Doctors use certain tests to determine if you have celiac disease, including:
- Blood tests – Also referred to as a celiac panel, this blood work searches for elevated levels of antibodies (infection-fighting cells). If you have celiac disease, higher than normal amounts of these cells indicate an immune reaction to gluten. Blood tests are typically the first step in celiac disease diagnosis.
- Endoscopy – An endoscopy (biopsy) is considered the “gold standard” for determining if you have celiac disease. During a biopsy, a long, thin tube (endoscope) with tools attached is passed through your digestive tract into your small intestine. These tools remove a tissue sample that will be analyzed in a lab to see if the villi have been damaged.
- Capsule endoscopy – During a capsule endoscopy, you swallow a pill-sized capsule containing a tiny, wireless camera. The capsule travels through your digestive tract while the camera takes thousands of pictures that are transmitted to a recording device worn on your body. These pictures will help your doctor analyze your small intestine.
Your doctor may also order the following:
- Blood tests that analyze other parts of your immune system.
- A blood count that looks for anemia (low red blood cells).
- Liver and kidney function tests.
- Tests that determine if there are vitamin D, B12, or folate deficiencies.
- If you have a rash, your doctor may take a skin sample to rule out other skin issues.
- Genetic testing that looks for human leukocyte antigens (key molecules in the immune response) to rule out celiac disease.
It’s very important that you don’t start a gluten-free diet before testing. If you stop eating gluten, your antibodies that fight it will drop, and your intestine will start healing, risking a false negative result. Your doctor may put you on a “gluten challenge,” a medical regimen during which you intentionally eat foods containing gluten. This may be four slices of wheat-based bread a day. After four to eight weeks, your doctor will analyze your blood for gluten antibodies.
Celiac Disease Treatment
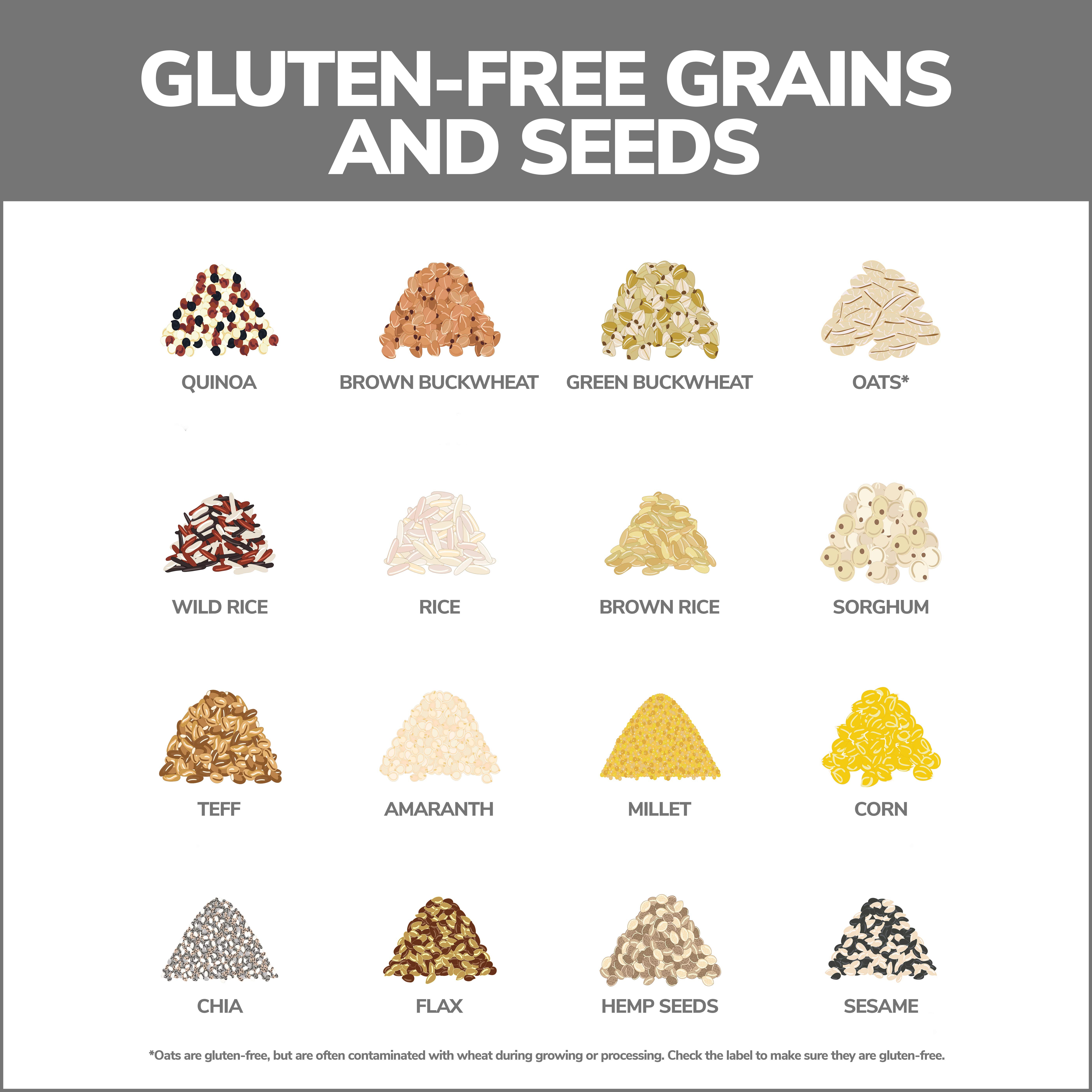
The only treatment for celiac disease is to stop eating gluten. When you stop eating gluten, your symptoms will probably improve in several days. Your small intestine should completely heal in three to six months, and your villi will resume absorbing nutrients. Most of the damage can be reversed. Your body may take a year or two to recover if you’re older.
Even if you’re feeling better, you’ll have to maintain a lifelong, gluten-free diet, so your symptoms aren’t re-triggered. Your doctor may refer you to a dietitian with expertise in celiac disease.
Foods to Avoid
Foods to avoid when you have celiac disease include:
- Beer, ale.
- Bread.
- Cakes and pies.
- Candies.
- Cookies and crackers.
- Dressings and condiments.
- French fries.
- Gravy.
- Hot dogs and processed meat.
- Hot and cold cereals.
- Ice cream.
- Matzo.
- Pastas.
- Potato chips and tortilla chips.
- Salad dressings.
- Soup, soup mixes.
How to Avoid Foods Containing Gluten When You’re Shopping
Many food labels will specify whether a product contains gluten or if it was made in a facility where gluten-containing goods are present. For example, a label may say, “Contains wheat, soy, egg, and milk ingredients.” Sometimes you may need to scrutinize labels listing alternative names for gluten or ones that aren’t easily recognizable, including:
- Wheat protein/hydrolyzed wheat protein.
- Hydrolyzed vegetable protein.
- Vegetable starch.
- Dextrin or maltodextrin.
- Modified starch.
- Seitan.
Gluten-containing ingredients may be listed under their Latin or scientific name. These include:
- Triticale.
- Hordeum vulgare.
- Triticum vulgare.
- Triticum spelta.
Some prescription and over-the-counter drugs and supplements may contain gluten as a binding agent, so talk to your doctor about your medications.
How to Maintain a Gluten-Free Diet When Eating Out
Removing gluten from your diet can be challenging and especially tricky when you’re eating out. There are guidelines you can follow to stay gluten-free in restaurants:
- Carry gluten test strips – Gluten test strips can determine if the food contains gluten.
- Limit the restaurants you go to – Find restaurants that have trustworthy gluten-free selections. You can also look up menus online before you go or speak to the staff about gluten-free dishes that they can provide. Find a restaurant that makes their food (or some dishes) from scratch, if possible.
- Don’t eat at fast food restaurants – Fast food restaurants are usually too frenzied to be able to talk about their food content.
- Eat at restaurants that are less hurried – These restaurants will be able to give you more attention and guidance in making appropriate selections.
- Call ahead – Call several hours before going to a restaurant and discuss your food options with the chef.
- Eat early or late – Time your meal before or after the restaurant’s rush hour. More people will be available, and they’ll be able to take more time to talk to you and prepare your special meal.
- Look for GFFS Safe Spots – Choose a restaurant that has gone through the Gluten Intolerance Group (GIG) Gluten-Free Food Services (GFFS) for restaurants. These restaurants have undergone extensive training and audits to learn how to prepare gluten-free food properly. After this, they are validated as Gluten-Free Safe Spots.
Contact Us
If you think you may have celiac disease, it’s important to get a diagnosis as soon as possible. Our practice began more than 15 years ago and has emerged as one of the leading gastroenterology practices in central Florida. We perform a host of diagnostic procedures using state-of-the-art equipment in a friendly, comfortable, and inviting atmosphere where patient care is always a top priority. Contact us today!