Chronic Pancreatitis
Chronic pancreatitis is a progressive disease that can permanently damage the pancreas and significantly impair a person’s quality of life. The condition can disrupt digestive processes, impact nutrition uptake, cause chronic pain, and lead to other serious complications.
Here we address the symptoms, causes, diagnosis, and treatment options for chronic pancreatitis.
What is Chronic Pancreatitis?
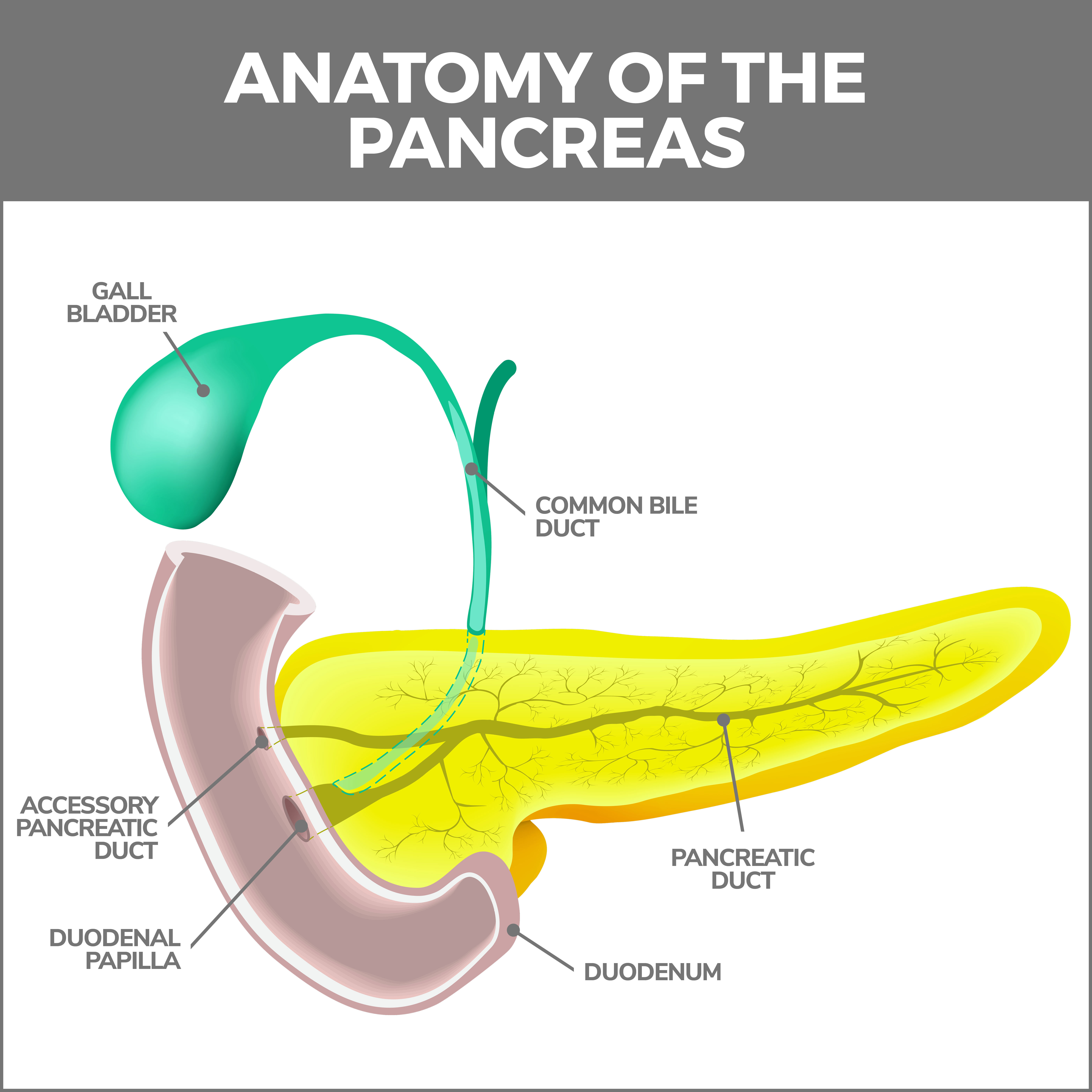
Chronic pancreatitis is a condition marked by long-standing inflammation of the pancreas, a vital organ nestled in the abdominal cavity, snug behind your stomach. This organ has two essential functions: 1. Aids digestion by secreting enzymes and 2. Helps regulate blood sugar levels by producing insulin. When persistent inflammation occurs, it can severely disrupt these functions and lead to various symptoms and complications.
Causes of Chronic Pancreatitis
Factors that may contribute to chronic pancreatitis include:
- Alcohol Consumption: Chronic pancreatitis, or long-term inflammation of the pancreas, is most often caused by drinking a lot of alcohol over a long time. It is not sure why this happens, but it seems that alcohol makes the pancreas create harmful substances that inflame and damage the pancreas cells. Alcohol can also make the tubes in the pancreas narrower, causing blockages. These blockages can build up pressure inside the pancreas and cause more harm.
- Genetic Factors: Certain gene changes inherited from parents can make some people more likely to develop chronic pancreatitis, a type of inflammation of the pancreas. For example, changes in a gene called PRSS1 can lead the pancreas to create an enzyme (a protein that helps our body perform various functions) that may start acting inside the pancreas rather than where it should – in the small intestine. When this happens, it can cause inflammation and damage to the pancreas. Another gene, SPINK1, typically helps control this enzyme. If this gene has changes or mutations, it might not keep the enzyme in check as effectively, leading to more harm to the pancreas. Lastly, changes in another gene, the CFTR gene, can disturb how fluids are produced in the pancreas, contributing to the chronic inflammation seen in pancreatitis.
- Autoimmune Conditions: Autoimmune pancreatitis is a rare disease where the body’s immune system mistakenly attacks the pancreas. This autoimmune response leads to pancreatic tissue inflammation and fibrosis (scarring). It’s often associated with other autoimmune conditions such as Sjogren’s syndrome, inflammatory bowel disease, and primary biliary cirrhosis.
- Obstructive Factors: Obstructing the central pancreatic duct can also lead to chronic pancreatitis. This can occur for various reasons, including pancreatic stones, tumors, or strictures (narrowing of the duct). These obstructions can block the outflow of pancreatic enzymes, leading to a buildup of pressure inside the pancreas, causing recurrent bouts of inflammation and, eventually, chronic damage.
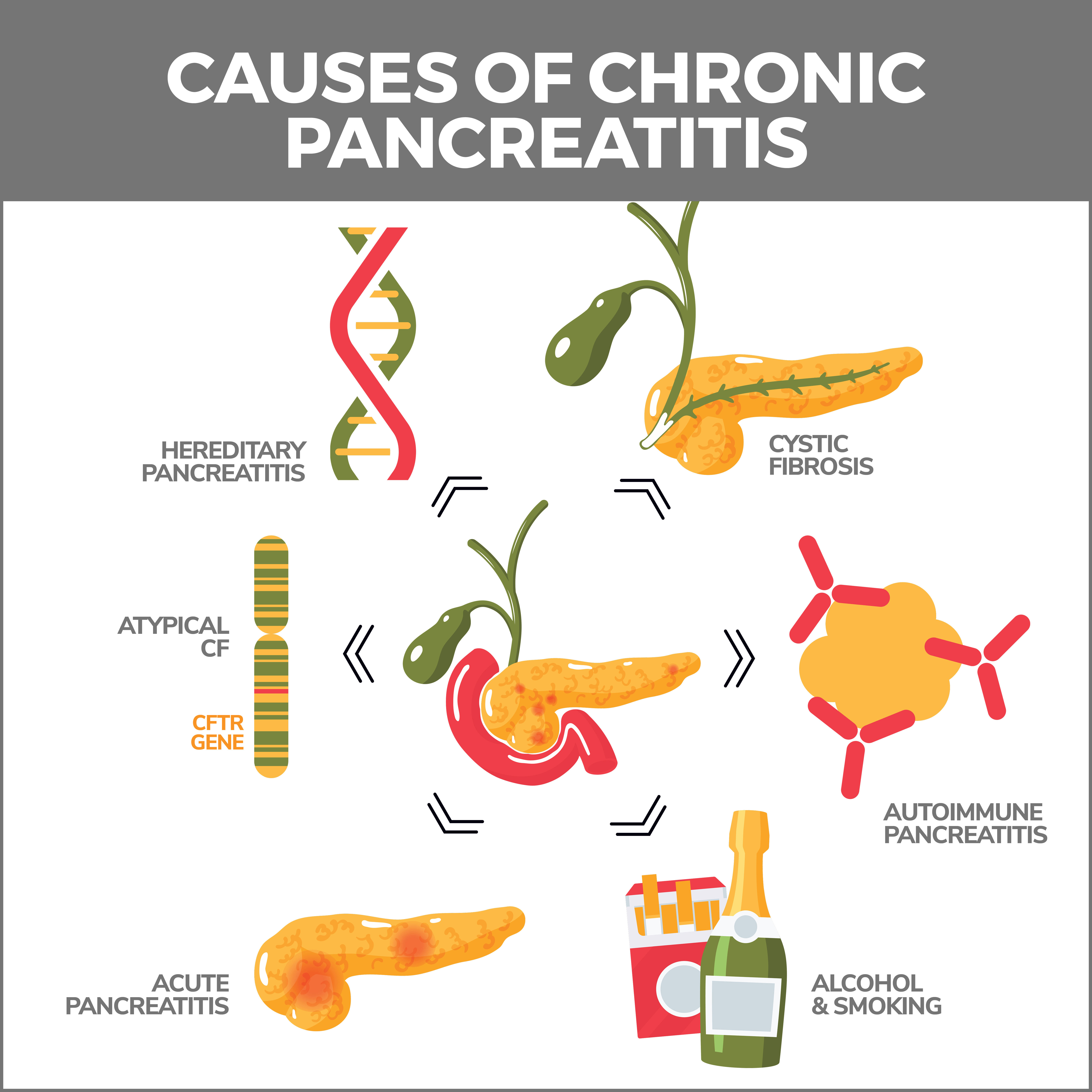
It’s important to note that while these are identified risk factors, chronic pancreatitis can still occur without these, because our understanding of the disease is still incomplete and ongoing. If you are experiencing persistent abdominal pain, loss of appetite, unexplained weight loss, or other symptoms related to chronic pancreatitis, please seek medical attention promptly.
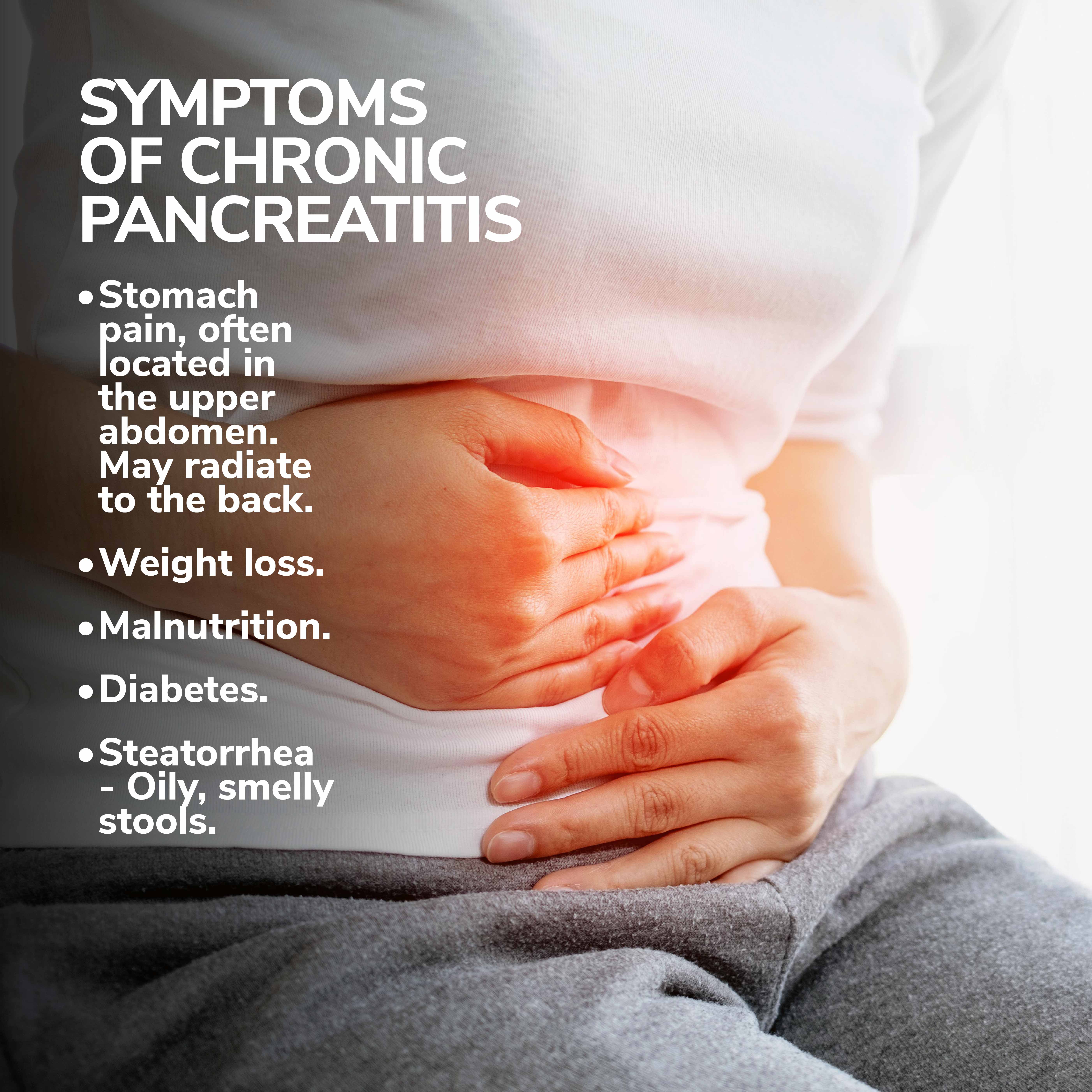
Symptoms of Chronic Pancreatitis
The primary symptom of chronic pancreatitis is stomach pain, which is often located in the upper abdomen and may radiate to the back. Other symptoms include:
- Weight Loss and Malnutrition: The pancreas produces enzymes that help digest food. Damage to the pancreas may result in poor absorption of nutrients, leading to weight loss and malnutrition.
- Diabetes: The pancreas also produces insulin, which regulates blood sugar levels. Damage to insulin-producing cells may lead to diabetes.
- Steatorrhea: Oily, smelly stools that are difficult to flush away. This occurs because the pancreas is not producing enough enzymes to break down fat.
Diagnosing Chronic Pancreatitis
The diagnosis of chronic pancreatitis is based on a patient’s history, symptoms, laboratory tests and imaging. There is no single test that is diagnostic of chronic pancreatitis, especially in the early stages. Each case of chronic pancreatitis has different contributing factors that influence the disease’s progression and severity.
Treating Chronic Pancreatitis
Managing chronic pancreatitis necessitates a multi-step approach. Your gastroenterologist can not only help to manage your symptoms but also prevent further damage to your pancreas.
Chronic pancreatitis is a progressive inflammatory disease that permanently damages the pancreas. This condition affects the pancreas’ ability to produce digestive enzymes and insulin, leading to digestive issues and diabetes. Here are a few ways to mitigate the risk of chronic pancreatitis:
Lifestyle Changes:
- Avoid Alcohol: Excessive alcohol consumption is one of the most common causes of chronic pancreatitis. If you’re at risk, it’s essential to either entirely abstain from alcohol or limit your intake to minimal levels.
- Dietary Adjustments: Adopting a low-fat diet can also make a significant difference. Consuming foods high in fats can exacerbate pancreatitis symptoms. Instead, choose a diet rich in fruits, vegetables, lean proteins, and whole grains.
- Hydration: Dehydration can negatively affect your pancreas, so drinking plenty of fluids throughout the day is crucial. This can include water, herbal teas, or other non-caffeinated, non-alcoholic drinks.
Medication:
If lifestyle changes aren’t enough, various medications can also help manage chronic pancreatitis symptoms and complications.
- Pain Management: Chronic pancreatitis often leads to severe pain. Doctors can prescribe analgesics – medications designed to reduce pain and improve quality of life.
- Enzyme Supplements: Because chronic pancreatitis can interfere with your body’s ability to digest food properly, doctors may recommend enzyme supplements. These supplements can assist in the breakdown of food – aiding digestion and nutrient absorption.
- Insulin Therapy: Chronic pancreatitis can sometimes lead to diabetes due to the pancreas’s role in insulin production. If this happens, insulin therapy may be required to help manage blood sugar levels.
Surgery:
- Clearing Blockages: Surgery can help clear blockages in the pancreatic duct, allowing digestive enzymes to move freely and reducing pancreas inflammation.
- Pancreas Surgery: In some instances, a part of the pancreas may need to be removed to manage symptoms and prevent further damage. This is typically a last resort when other treatment options have failed.
These steps and regular check-ups with your gastroenterologist can significantly reduce the risk of chronic pancreatitis or help manage its symptoms effectively. Everyone is different, so a treatment plan that works for one person might not work for another. Working closely with your doctor to find the best strategy for you is essential.
Contact Us
Chronic pancreatitis can significantly affect a person’s quality of life. Early diagnosis and prompt management are crucial. Our team of trusted experts can help you manage this condition effectively.
If you’re experiencing symptoms of chronic pancreatitis, don’t hesitate to contact Gastroenterology of Greater Orlando. Our practice began more than 15 years ago and has emerged as one of the leading gastroenterology practices in central Florida. We perform a host of diagnostic procedures using state-of-the-art equipment in a friendly, comfortable, and inviting atmosphere where patient care is always a top priority. Contact us today!