The Complete Guide to Anal Fissures
Anal fissures, often a topic that’s avoided, are a common medical condition that can affect individuals of all ages. These painful tears or cracks in the delicate lining of the anus that results in discomfort and distress. Their symptoms can be very uncomfortable and even debilitating.
In this blog, we will discover the causes behind anal fissures, explore the telltale signs and symptoms, and discuss the various treatments and preventive measures that can bring relief and restore well-being. Understanding this condition is the first step toward addressing it effectively.
Understanding Anal Fissures
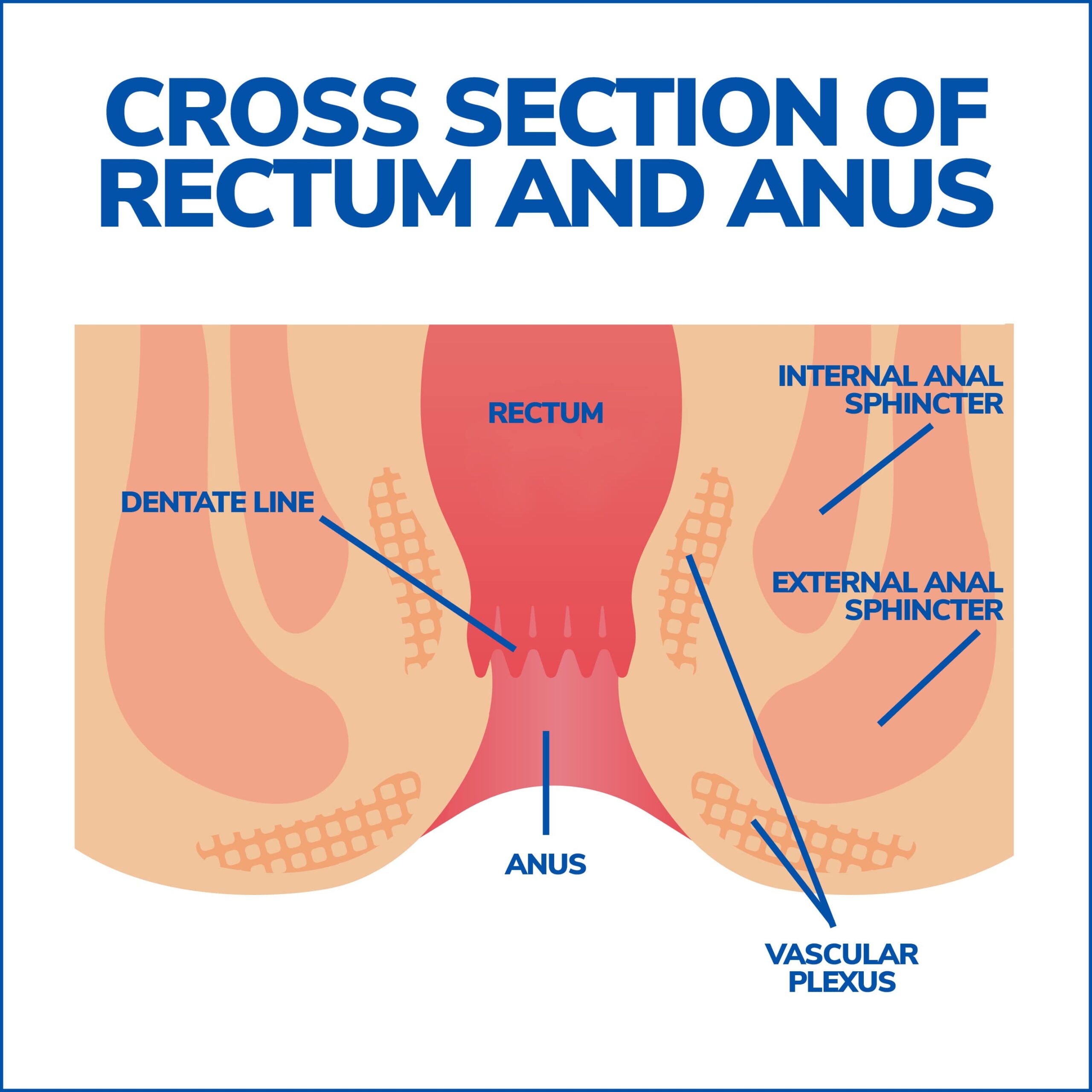
An anal fissure refers to a tear or open sore in the lining of the anus, also known as the anal mucosa. This condition can cause significant discomfort and pain, emphasizing the importance of seeking appropriate treatment and preventative measures.
Causes of Anal Fissures
Anal fissures often develop due to the stretching of the anal mucosa beyond its normal capacity. The most common cause is constipation, which leads to the passage of hard or large stools that can tear the lining of the anal canal.
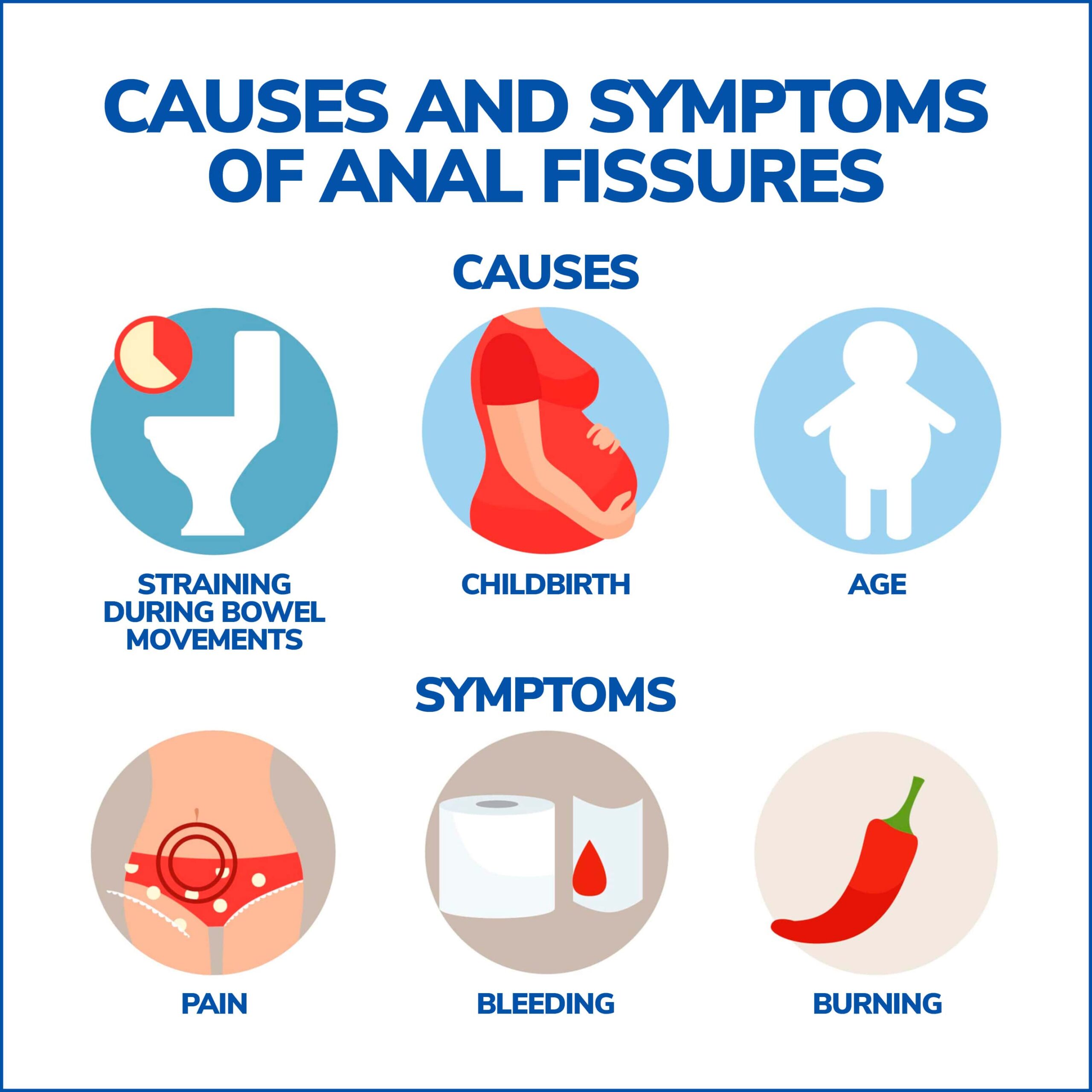
Anal fissures can be caused by various factors, including:
- Straining During Bowel Movements: Excessive straining while passing stool is a common cause of anal fissures. The extra pressure can lead to tears in the anal lining.
- Hard or Large Stools: Constipation, or the passage of hard, large stools, can stretch and injure the anal mucosa, increasing the risk of fissures.
- Diarrhea: Frequent and watery bowel movements can irritate the anus, potentially leading to the development of fissures.
- Childbirth: Anal fissures can occur during childbirth due to the pressure and stretching of the anal canal.
- Anal Trauma: Injury or trauma to the anal area, such as from anal intercourse or the insertion of foreign objects, can result in fissures.
- Anal Conditions: Certain underlying conditions like hemorrhoids or inflammatory bowel disease (IBD) can contribute to the development of anal fissures.
- Infections: Infections in the anal area can cause inflammation and tissue damage, potentially leading to fissures.
- Age: Anal fissures can affect people of all ages but are primarily found in infants and older adults.
Identifying Symptoms
Recognizing the symptoms of anal fissures is crucial for prompt diagnosis and treatment. The most common symptoms include sharp pain during bowel movements, followed by a deep burning pain that can last for several hours. Additionally, individuals may notice bright red blood in their stools or on the toilet paper.
Symptoms of anal fissures may include:
- Pain: The most common symptom is sharp, stabbing, or burning pain during or after bowel movements.
- Bleeding: Bright red blood may be seen on toilet paper or in the toilet bowl after a bowel movement.
- Itching: The area around the anus may become itchy due to irritation.
- Tenderness: The skin around the anus can be tender to the touch.
- Spasms of the Anal Sphincter: Some individuals experience spasms of the anal sphincter muscles, which can intensify pain and hinder healing.
- Discomfort: A constant feeling of pain or a feeling of fullness in the anal area.
- Fecal Leakage: In some cases, anal fissures can lead to difficulty controlling bowel movements, resulting in minor fecal leakage.
If you suspect you have an anal fissure or are experiencing these symptoms, it’s essential to consult a gastroenterologist for proper evaluation and treatment. Do not let embarrassment hinder you from seeking help, as anal fissures are a common problem that they are accustomed to addressing.
Diagnostics and Treatment Options
Diagnosing and treating anal fissures requires a multifaceted approach, aimed at relieving discomfort and promoting the healing process. Doctors typically diagnose anal fissures through a physical examination and a review of symptoms. A proper diagnosis is necessary to rule out other conditions with similar symptoms, such as hemorrhoids.
Diagnosing Anal Fissures
To diagnose an anal fissure, your gastroenterologist will inquire about your symptoms and conduct a visual examination of the affected area. In some cases, a digital rectal examination may be necessary. In certain situations, further tests or specialist assessments may be required.
Conservative Treatment Options
Most anal fissures can heal without the need for invasive treatments. Conservative approaches are often recommended initially and may include dietary modifications to increase fiber intake, staying hydrated, and adopting regular bowel habits. These measures aim to promote softer stools and relieve strain during bowel movements.
Medication and Topical Treatments
In cases where conservative measures are insufficient, your gastroenterologist may prescribe medication and topical treatments. Laxatives can help ease bowel movements, while pain-relieving ointments can provide temporary relief. There are also medications available that improve blood flow to the affected area, aiding in the healing process.
Surgical Interventions
When conservative treatments and medications fail to resolve chronic anal fissures, surgical interventions may be considered. Surgical options include lateral internal sphincterotomy, a procedure that involves releasing the pressure inside the anus to promote healing. It is important to note that surgery carries potential risks, such as infection or temporary loss of bowel control.
Preventing Anal Fissures
Prevention is key to avoiding the recurrence of anal fissures. Simple lifestyle changes can significantly reduce the risk of developing this condition. These include maintaining a high-fiber diet, staying hydrated, exercising regularly, and not ignoring the urge to have a bowel movement. By following these guidelines, you can promote regular and healthy bowel habits.
Living with Anal Fissures
Living with anal fissures can be challenging, but there are ways to manage the condition and improve your quality of life. It is important to adhere to prescribed treatments and self-help measures. You can reduce pain and discomfort by using over-the-counter painkillers, taking warm baths, and avoiding spicy foods that may worsen symptoms.
Complications and Recurrence
While most anal fissures heal within a few weeks, some cases may become chronic or reappear. Chronic (long term) anal fissures can lead to complications such as reduced quality of life and difficulty with bowel movements. Monitor your symptoms and seek medical attention if complications arise or symptoms persist beyond the expected healing period.
Contact Us
Anal fissures can be a distressing condition, but with the right knowledge and proper treatment, individuals can find relief. By understanding the causes, recognizing symptoms, and seeking medical attention, you can start on a path toward recovery and minimizing future occurrences.
Contact Gastroenterology of Greater Orlando today for a comprehensive evaluation, diagnosis, and personalized treatment options to ensure your continued well-being and comfort. Don’t allow anal fissures to disrupt your quality of life. Instead, take proactive measures towards a healthier and more comfortable lifestyle.