
Breaking Down FODMAPs: Managing Food Sensitivities
For many people, certain foods can trigger uncomfortable digestive symptoms like bloating, gas, and changes in bowel habits. These problematic foods are often high in FODMAPs. FODMAP, an acronym for fermentable oligosaccharides, disaccharides, monosaccharides, and polyols, refers to a group of carbohydrates that can be difficult for some individuals to digest. Knowing FODMAPs is key for those with IBS or gut issues. A specialized diet to manage them can be life-changing.
Understanding FODMAPs
High-FODMAP foods can cause unpleasant symptoms in many people. This is especially true for those with irritable bowel syndrome (IBS) and other digestive disorders. These symptoms may include bloating, gas, abdominal pain, and changes in bowel movements. The low-FODMAP diet helps people find and manage food sensitivities. It does this by removing high-FODMAP foods and then gradually reintroducing them to find triggers.
FODMAPs can cause discomfort in some people when they ferment in the gut. When undigested, these carbohydrates reach the large intestine. There, they attract water and are rapidly fermented by gut bacteria. This fermentation process produces gas, which can lead to bloating, abdominal pain, and changes in bowel movements. For those with IBS or SIBO, this fermentation can worsen symptoms and cause pain.
FODMAP Categories
There are four main categories of FODMAPs, each containing specific types of carbohydrates:
- Oligosaccharides: This category includes fructooligosaccharides (FOS) and galactooligosaccharides (GOS). FOS is found in foods like onions and garlic, while GOS is primarily found in legumes. Both can promote gut health but may cause discomfort in sensitive individuals.
- Disaccharides: These refer mainly to lactose, which is found in milk and dairy products. As people age, they produce less lactase, which can cause lactose intolerance, with symptoms like bloating and diarrhea.
- Monosaccharides: Primarily fructose, found in fruits and honey. Excess fructose can cause gastrointestinal symptoms when not balanced by glucose.
- Polyols: Sugar alcohols like sorbitol and mannitol are found in certain fruits and sugar-free products. In larger amounts, they can lead to digestive discomfort.
The Low FODMAP Diet Explained
The low FODMAP diet helps people with food sensitivities. This diet involves three phases: elimination, reintroduction, and personalization.
- Elimination Phase: This stage involves avoiding all high-FODMAP foods for 2-6 weeks. During this time, individuals eat only low-FODMAP foods. This calms the gut and improves symptoms.
- Reintroduction Phase: After symptoms stabilize, reintroduce foods from each FODMAP category one at a time. This process helps identify which specific FODMAPs trigger symptoms and in what quantities.
- Personalization Phase: Based on the reintroduction phase, individuals can now create a long-term diet. It should exclude problematic FODMAPs and reincorporate well-tolerated foods.
This three-step approach alleviates digestive discomfort and empowers individuals to make informed dietary choices for better gut health. Consulting with a doctor or registered dietitian is recommended to ensure proper implementation and nutritional balance.

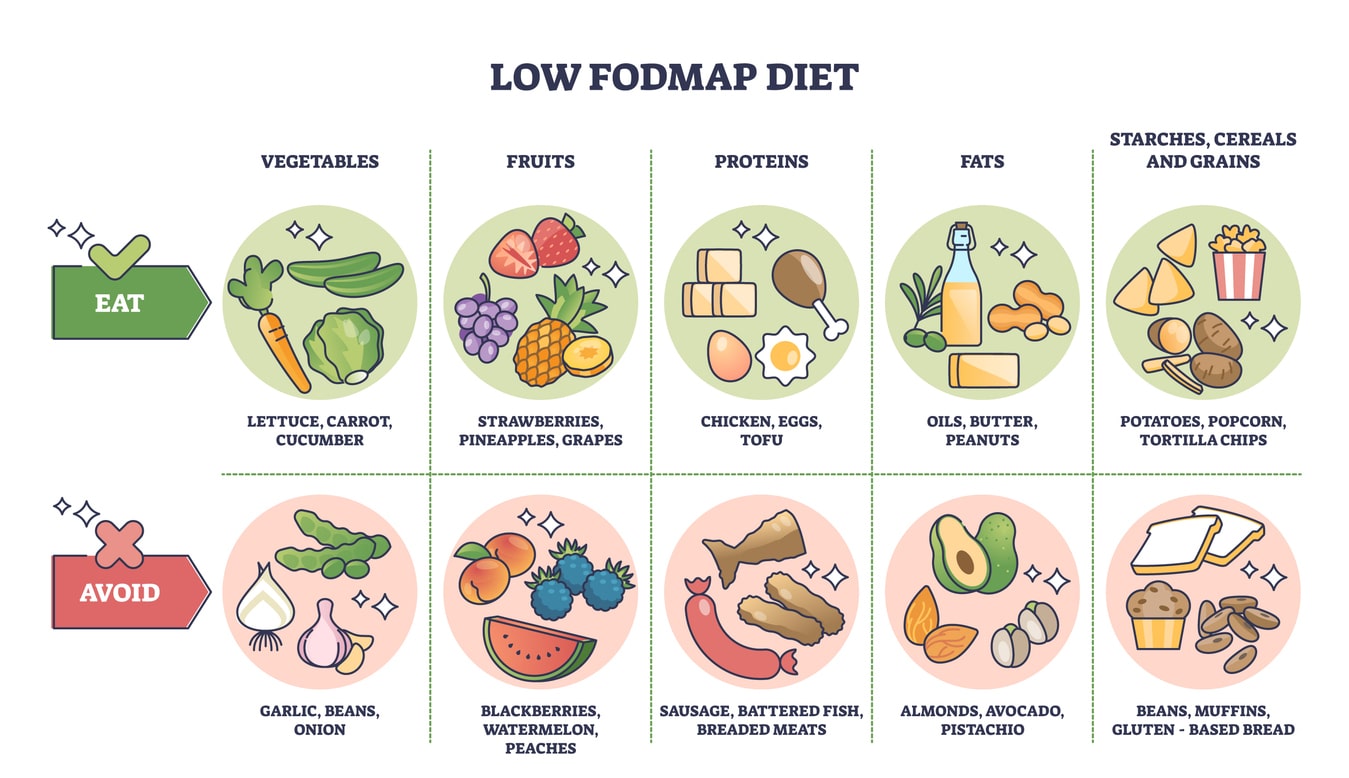
Low FODMAP Foods to Enjoy
A low FODMAP diet includes many satisfying, nutrient-rich foods. They are easy on the digestive system and work well in daily meals. Consider the following options:
- Fruits: Enjoy low-FODMAP fruits like bananas, blueberries, and strawberries. They are sweet but won’t upset your stomach.
- Vegetables: Carrots, spinach, and zucchini are nutrient-dense, low-FODMAP veggies. They are ideal for this diet.
- Proteins: Chicken, turkey, and fish are FODMAP-free. They can be used in many meals to support balanced nutrition.
- Grains: Rice, quinoa, and oats are low-FODMAP, filling options. They are easy on the stomach and versatile in recipes.
- Dairy Alternatives: Almond milk and lactose-free yogurt are creamy. They are good for meals and snacks. They are alternatives to dairy, with no digestive issues.
High FODMAP Foods to Limit
To manage digestive symptoms, avoid certain foods to improve comfort and well-being.
- Fruits: Avoid high-FODMAP fruits like apples, pears, and cherries, as these can sometimes cause digestive discomfort.
- Vegetables: Vegetables such as cauliflower, garlic, and onions are high in FODMAPs and can contribute to bloating and gas.
- Proteins: Processed meats, such as sausages and certain deli meats, often contain high-FODMAP additives, so it’s helpful to monitor these options.
- Grains: Foods like wheat, rye, and barley are high in FODMAPs and may trigger symptoms, especially in larger quantities.
- Dairy Products: Regular milk, ice cream, and soft cheeses contain lactose, a high-FODMAP component that is hard to digest for many people.
Key Considerations for Managing FODMAPs
It’s important to note that serving size plays a significant role in FODMAP content. Some foods may be tolerated in small amounts but become problematic in larger quantities. Food processing can affect FODMAP levels. For example, while fresh apples are high in FODMAPs, small amounts of apple cider vinegar may be well-tolerated due to fermentation.
It’s crucial to read food labels carefully when following a low-FODMAP diet, especially during the elimination phase. Many processed foods have hidden FODMAPs. These include inulin (a fructan) and high-FODMAP ingredients like onion and garlic powders. Being vigilant about ingredient lists can help avoid unintentional FODMAP consumption.
It’s also worth noting that some foods can be high in multiple FODMAP types. For instance, apples contain excess fructose and sorbitol, while wheat contains fructans and galacto-oligosaccharides. This overlap can make certain foods particularly problematic for sensitive individuals.
Remember, the goal of identifying high-FODMAP foods is not to eliminate them permanently from your diet. It’s to understand your tolerances and create a sustainable eating plan that minimizes symptoms while maximizing dietary variety and nutritional intake.
Easing Into a Low FODMAP Lifestyle
At first, a low FODMAP diet may seem challenging. Here are five helpful tips to ease your journey:
- Plan Ahead: Prepare meals in advance to avoid impulsive choices and ensure you have suitable options available.
- Educate Yourself: Learn which foods are high and low in FODMAPs and keep a handy list for shopping and meal planning.
- Read Labels: To avoid accidental consumption, check ingredient lists for hidden FODMAPs, like inulin or garlic powders.
- Start Gradually: Begin with one low FODMAP meal daily to ease the transition without feeling overwhelmed.
- Seek Support: Connect with a registered dietitian for personalized guidance and reassurance throughout the process.
Navigating the Path to Digestive Relief with FODMAPs
A low-FODMAP lifestyle takes some adjustment but can help with digestive issues if you use the right strategies. By understanding FODMAP categories, identifying your triggers, and gradually incorporating low-FODMAP foods, you can take control of your gut health and relieve troubling symptoms.
If you have persistent digestive issues, the Gastroenterology of Greater Orlando team can help. With a personalized approach, we will work closely with you to develop an effective management plan that allows you to reclaim your digestive health and quality of life. Contact Gastroenterology of Greater Orlando and take the first step towards better gut health.