Ulcerative Colitis Condition
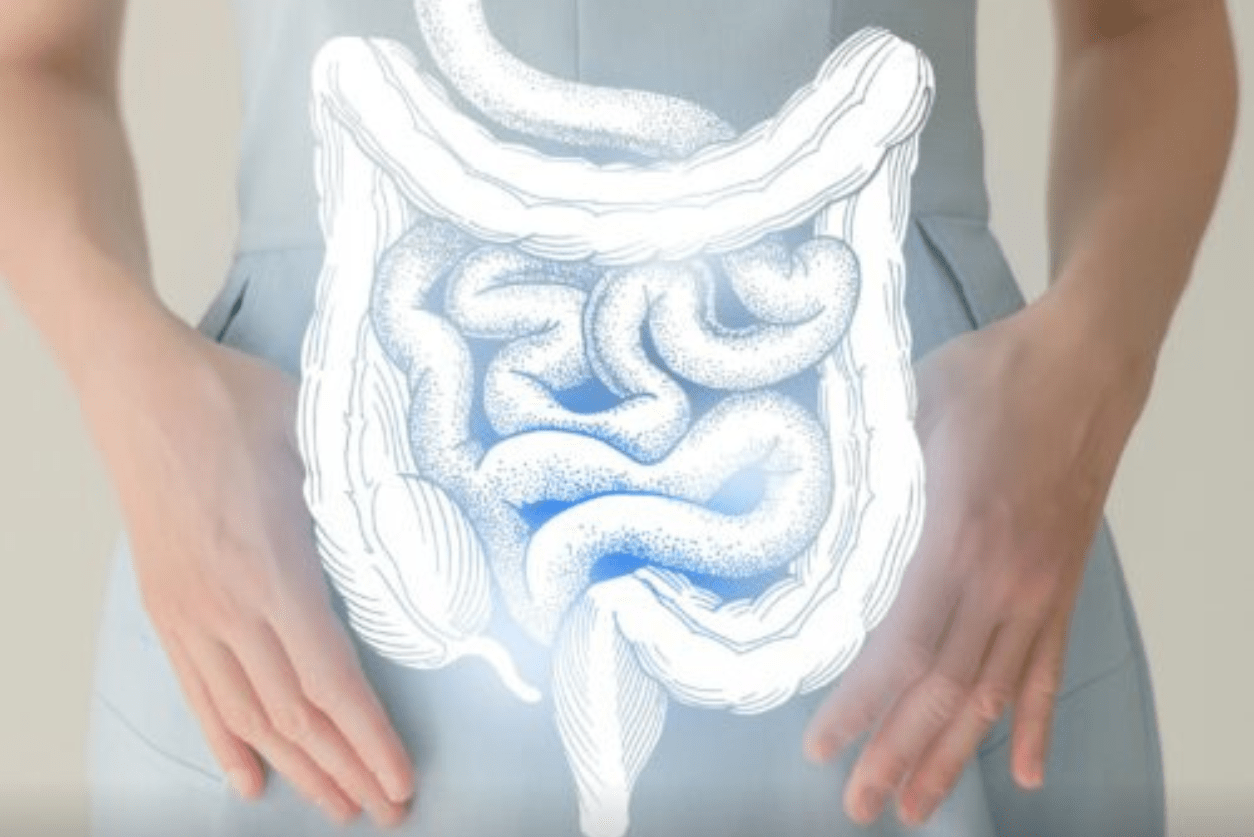
Your gastrointestinal tract carries out the vital functions of breaking down the foods you eat, processing the crucial nutrients contained inside such products, and eliminating potentially harmful waste products. A key component of this network is the large intestine, which is known as the colon.
Many diseases can disrupt these vital functions and cause bothersome and sometimes serious problems. One such issue is ulcerative colitis condition.
Ulcerative Colitis
Ulcerative colitis is what medical professionals label an inflammatory bowel disease.
The disorder is categorized by the development of painful ulcers throughout your colon. Incidents of the disease typically occur in what are called flares. This means symptoms gradually emerge and linger for weeks or even months at a time, stop for lengthy periods, and then ultimately appear again.
Types
The ulcerative colitis condition is divided into four types, including:
- Left-Sided Colitis: This variation impacts the sigmoid (lower reaches of your colon and rectum). The inflammation remains strictly on the organ’s left side.
- Ulcerative Proctitis: This form of the disease impacts only the anal region.
- Proctosigmoiditis: This form of the disease strikes the sigmoid colon and rectum.
- Pancolitis: Pancolitis impacts the entire organ.
Causes
Researchers have been unable to pinpoint any one specific cause. They believe abnormal immune system function is a major contributing factor. Some believe the immune system is triggered by any number of pathogens (bacteria, viruses, or other microorganisms that can cause disease). Instead of merely attacking the pathogens, immune network cells also attack the colon.
Risk Factors
Many factors increase your risk of contracting the ulcerative colitis condition, including:
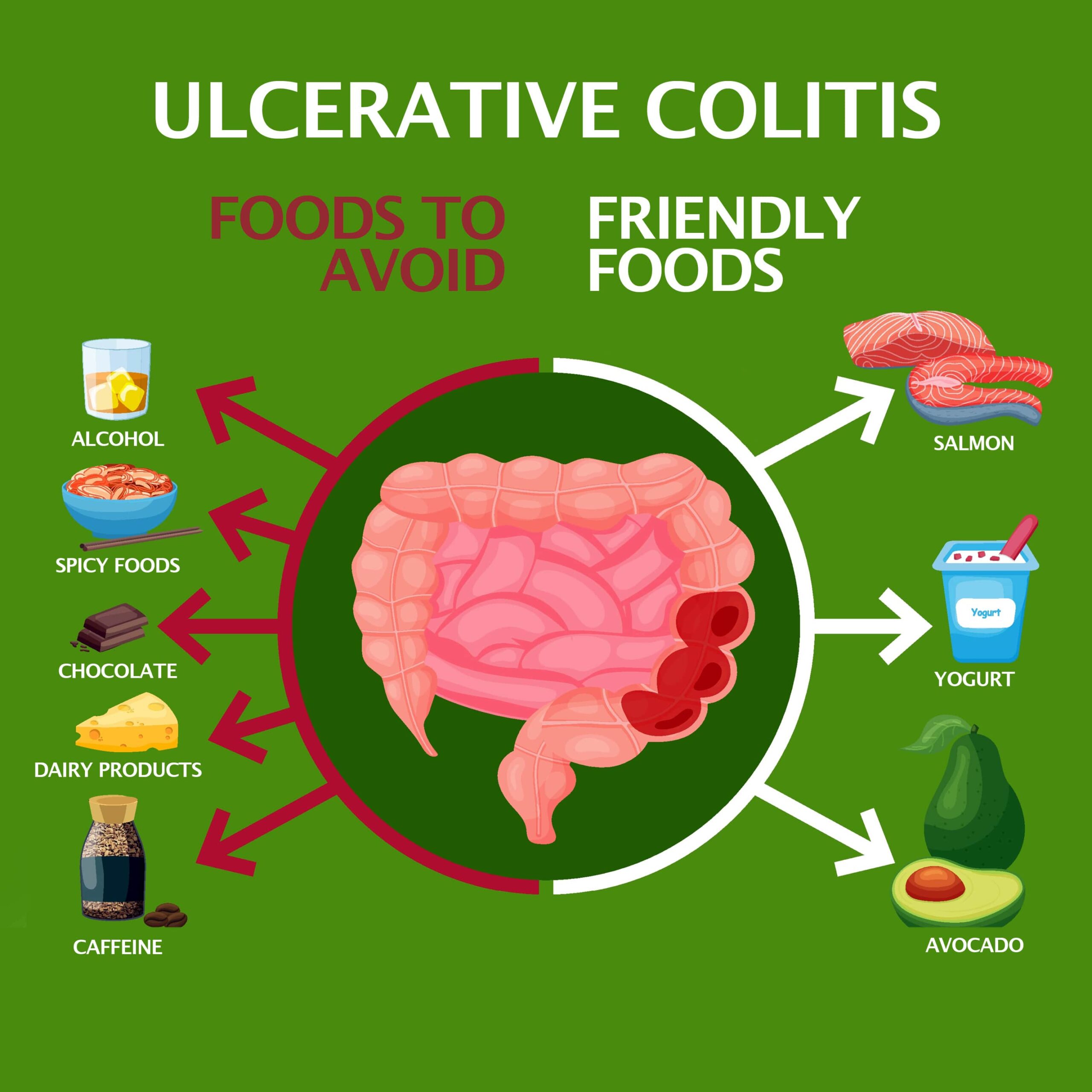
- Diet: The consumption of overly processed, spiced, frozen, or canned goods may increase your chances. Additionally, your risk heightens if you eat large quantities of fat.
- Vices: Vices like cigarette smoking and excessive alcohol intake have been known to irritate the gastrointestinal tract lining.
- Stress: Continual exposure to stress often exercises a negative influence on the digestive system.
- Age: In many instances, the ailment impacts individuals between 15 and 30. But you can be stricken at any age.
- Ethnicity: Ethnic background plays a significant role. Researchers have found that persons of Ashkenazi Jewish ancestry are more likely to develop the problem than those of other faiths and backgrounds.
- Family History: Your risk elevates if you have a close family member diagnosed with the illness. Researchers have found that persons with parents or siblings with ulcerative colitis or other inflammatory bowel disease are far more likely to contract the disorder.
- Use Of Specific Medications: Your chances of getting ulcerative colitis increase dramatically if you frequently take over-the-counter medications known as non-steroidal anti-inflammatory drugs. These substances, often abbreviated as NSAIDs, are believed to irritate the colon’s lining.

Symptoms
The symptoms you encounter often depend on the specific type of disease you have. The ulcerative colitis condition often produces generalized symptoms, including:
- Blood in the stools.
- Loose stools or full-blown diarrhea.
- Abdominal cramping.
- The urge to defecate frequently.
- Bloating.
- Loss of appetite.
Serious or progressive cases might also precipitate more significant symptoms such as:
- Weight loss.
- Anemia.
- Fatigue.
- Elevated body temperature.
Complications
If left unchecked, the ulcerative colitis condition can lead to potentially serious complications such as:
- Colon scarring.
- Dehydration.
- Inflammation in your skin, joints, and eyes.
- Dangerous internal blood loss.
- Colon perforation.
- Toxic megacolon.
- Bowel obstruction.
Long-standing colitis heightens your risk for colon cancer development.
Diagnosis
Diagnosis is often a multi-pronged process. During the first phase, doctors will offer a thorough physical examination. Your provider might ask you about your dietary habits, if you smoke or drink, the amount of stress you are exposed to, your symptoms, and if anyone in your family has been diagnosed with some type of inflammatory bowel disorder.
If your doctor thinks you may have the ulcerative colitis condition, they may then order a variety of tests, including:
- Blood Work: Blood tests enable doctors to rule out other conditions. Ulcerative colitis often mimics other potentially hazardous illnesses like cancer.
- Internal Imaging Tests: Internal imaging tests may be used to confirm the diagnosis. Such tests include colonoscopy, sigmoidoscopy, and computerized tomography. These apparatuses enable doctors to view inside your colon and identify any noticeable abnormalities.
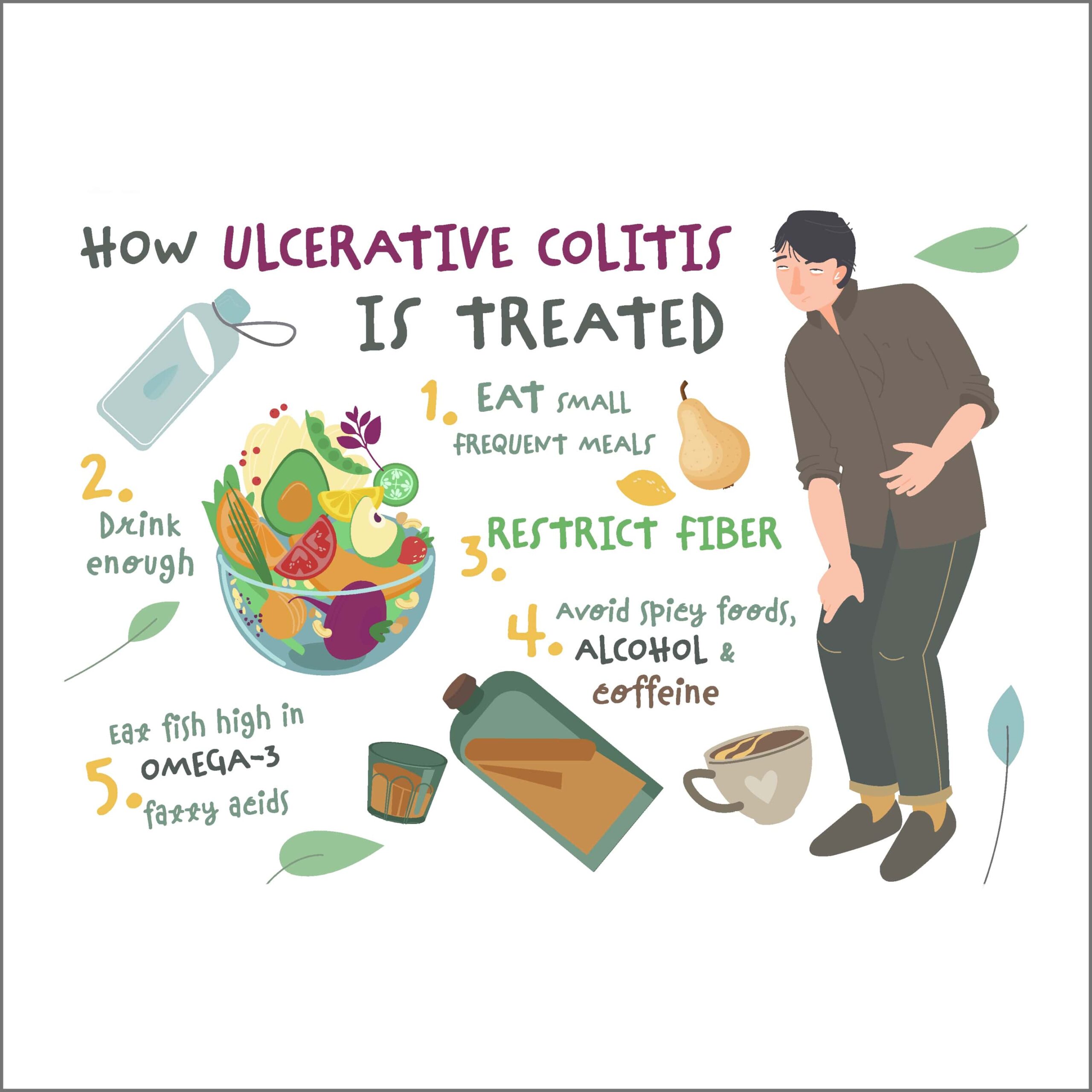
Treatment Options
Ulcerative colitis is a chronic condition for which there is no cure. Treatment options are available. The specific therapy employed by your doctor will depend on the severity, its location within your colon, your age, and general health.
Commonly utilized treatment methods include:
- Natural Remedies: Milder cases may improve using natural methods such as probiotics and various herbal supplements to soothe the digestive tract. Other natural efforts known to yield beneficial results include limiting stress, consuming a healthy and balanced diet, limiting or quitting vices like drinking and smoking, and regulating your intake of NSAIDs.
- Medications: Various drugs have proven effective in lessening symptoms and expediting flare-ups. Such drugs include anti-inflammatory agents and biological substances, which are believed to inhibit the immune system’s ability to produce inflammation.
- Surgery: Surgery may be required in severe cases or when the disease has produced significant complications. Such interventions may be used to remove a part of damaged tissue. In the most serious cases, the entire colon might need extraction.
Recovery
Mild flares often dissipate on their own. More significant events typically need more aggressive treatment. The duration of each flare will depend on the individual and their response to a given treatment. You can live with the disease for many years with proper individual and medical oversight.
Contact Us
Our practice began more than 15 years ago and has emerged as one of the leading gastroenterology practices in central Florida. We perform a host of diagnostic procedures using state-of-the-art equipment in a friendly, comfortable, and inviting atmosphere where patient care is always a top priority. Contact us today!