Everything to Know About the Gut-Brain Axis
Emerging research sheds light on the intricate relationship between our gut and our brain. The “gut-brain axis,” a term coined to describe this connection, impacts many aspects of our lives – from mood and mental health to metabolism and overall well-being. Understanding the complexity of the gut-brain link can help you take better care of your health.
Issues with the gut-brain connection can dramatically affect our physical and mental health. It is important to understand this link to prevent potential health complications and improve our overall well-being.
What is the Gut-Brain Axis?
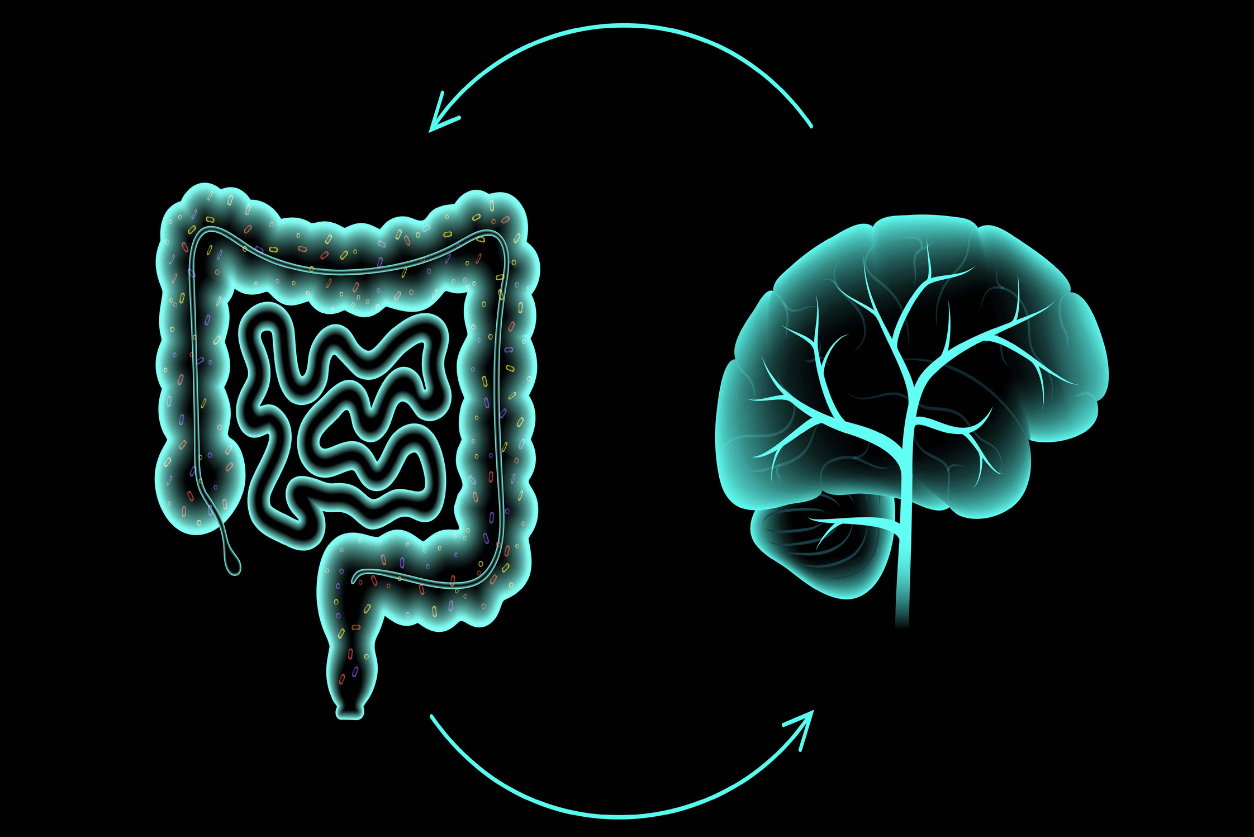
The gut-brain axis (GBA) is the communication network connecting your gut and brain. These two organs are physically and biochemically connected in several ways. This intricate, bi-directional communication system ensures the proper maintenance of gastrointestinal stability (homeostasis) and impacts higher intellectual activity, including mood and behavior.
Components of the Gut-Brain Axis
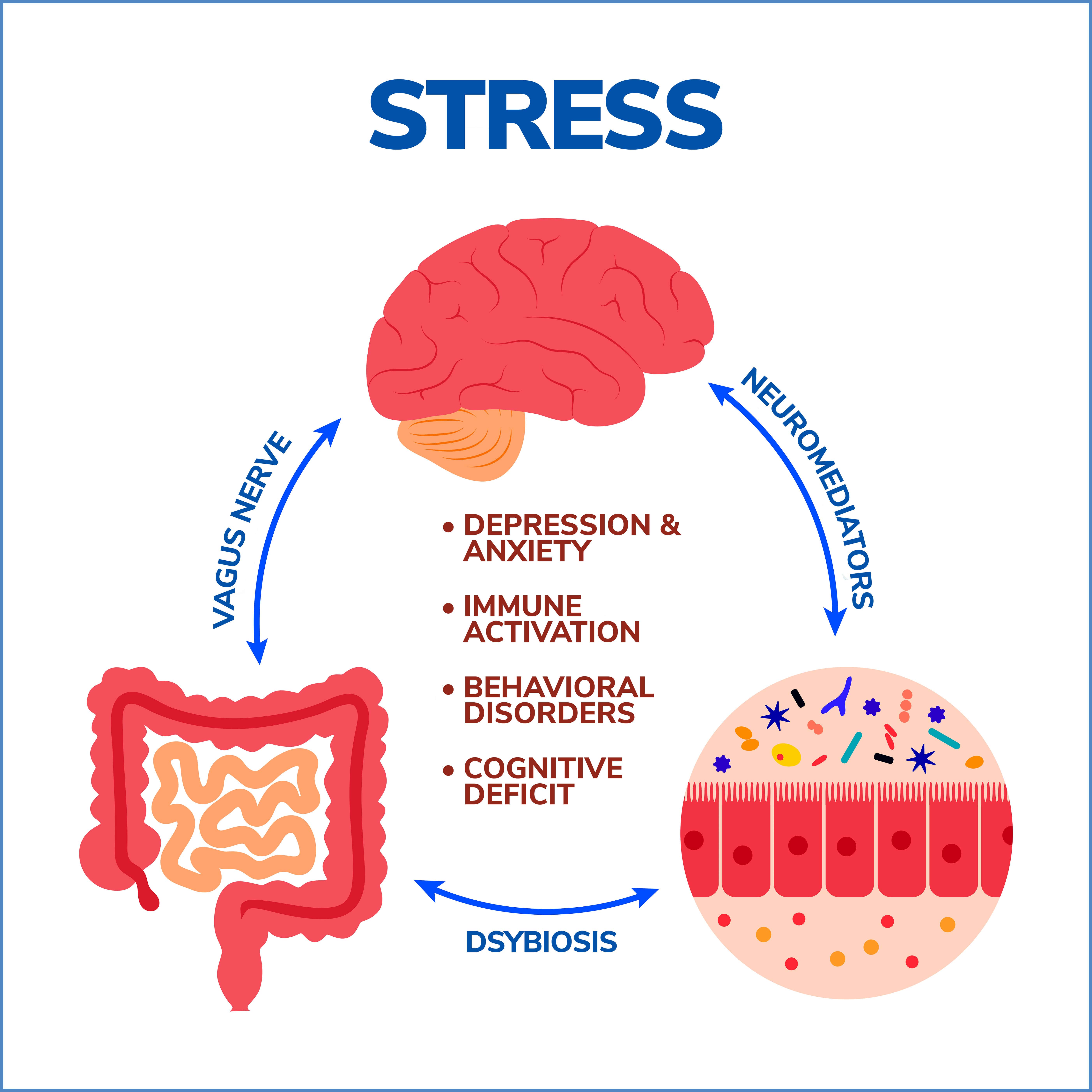
- Vagus Nerve: The vagus nerve is a critical component of the gut-brain axis, serving as a primary highway for information exchange between the gut and the brain. This cranial nerve extends from the brainstem to the abdomen, providing two-way communication between these organs.
- Hormones and Neurotransmitters: The gut and the brain communicate using several signals, including hormones and neurotransmitters. The gut itself produces many substances that can affect the brain. For example, about 90% of the body’s serotonin, a neurotransmitter that contributes to happiness and well-being, is produced in the gut.
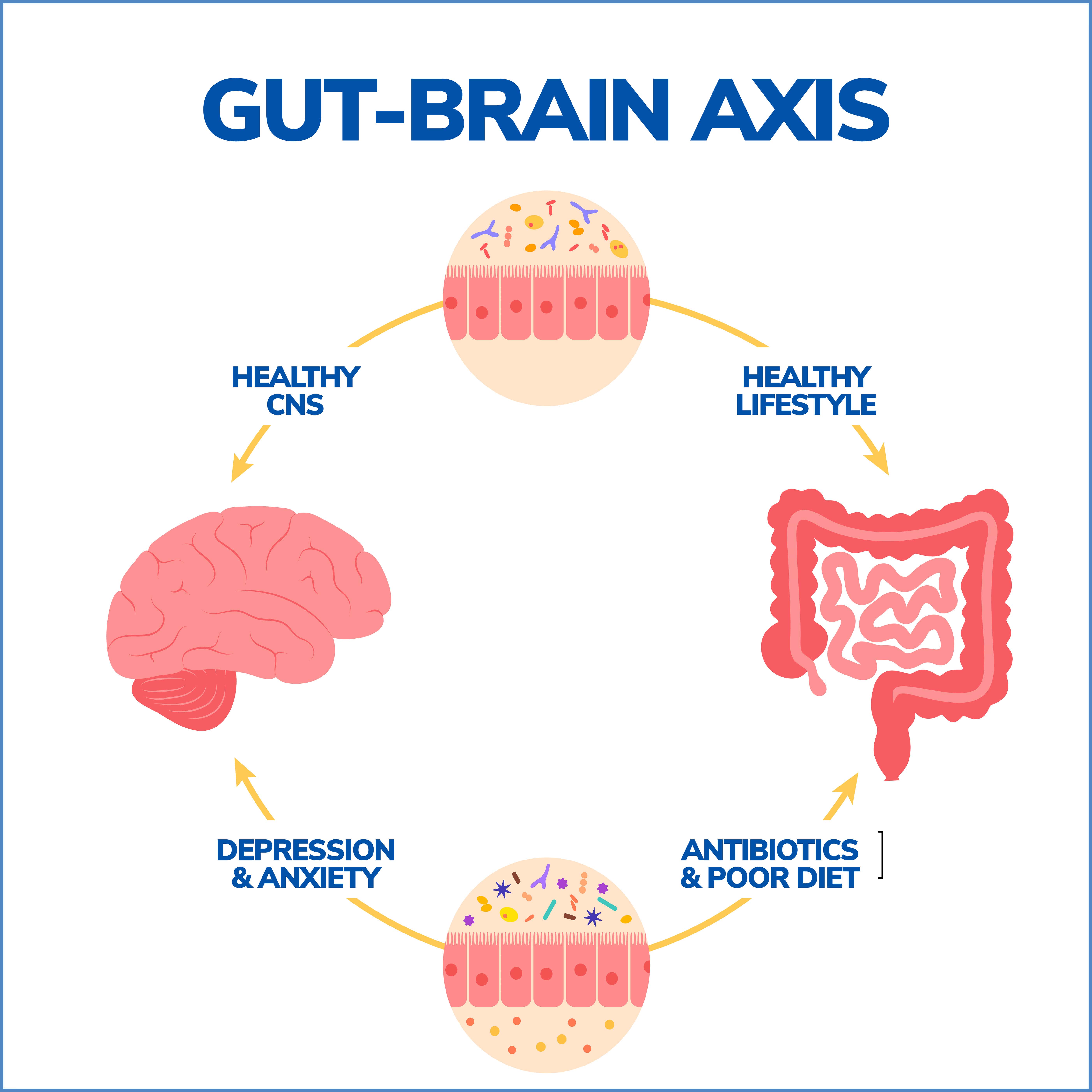
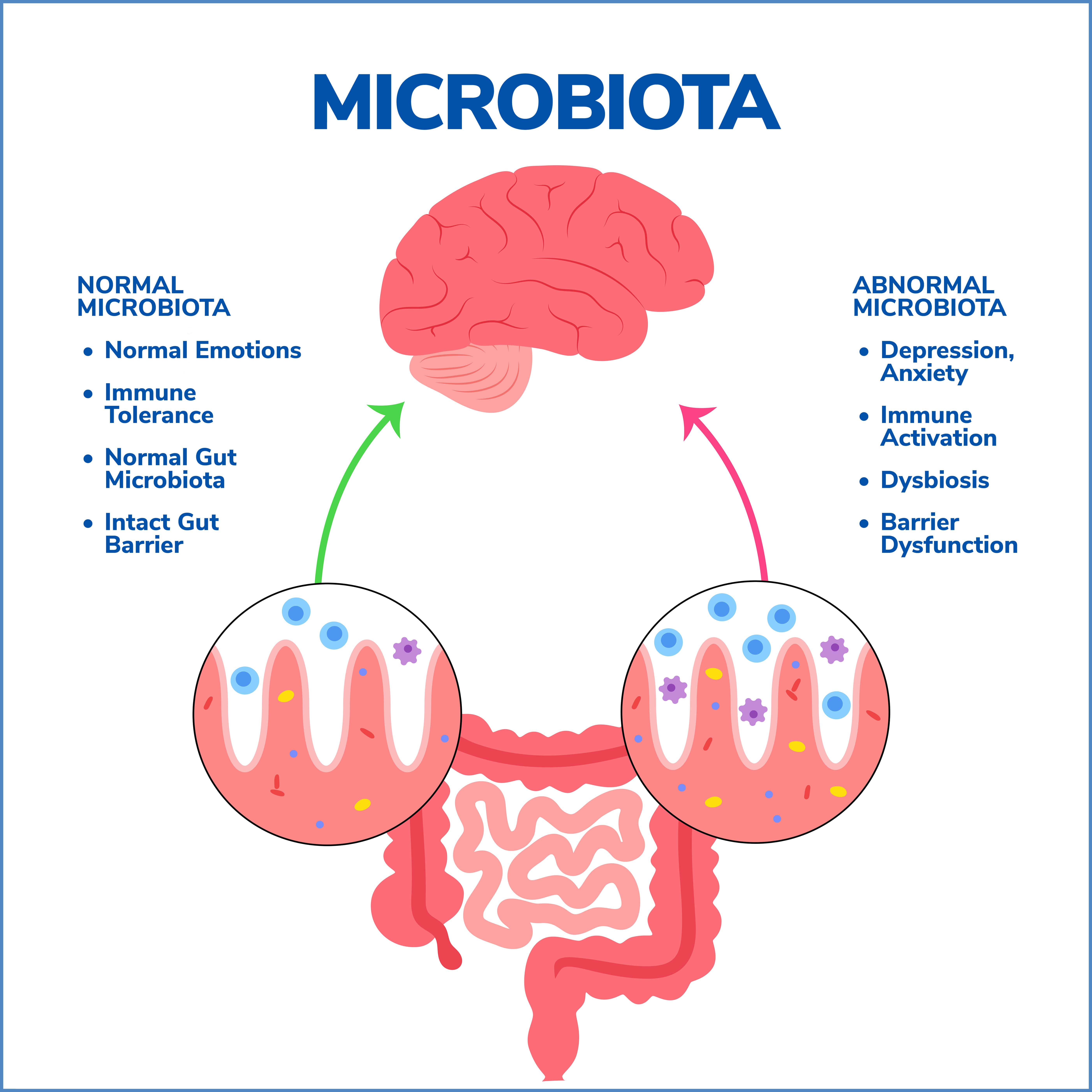
- Gut Microbiome: Your gut is home to trillions of microbes (collectively, the gut microbiome), which play an essential role in your health by helping digest food, synthesizing vitamins, and protecting against disease-causing organisms. The gut microbiome can also affect the brain and influence behavior. This is sometimes referred to as the microbiota-gut-brain axis.
How Does the Gut-Brain Axis Impact Health?
The gut-brain axis – a complex communication network between the gut and brain – is increasingly recognized as critical in maintaining overall health. A bi-directional system allows the brain to influence gut activities and gut functions to impact brain health. Disruptions in this finely-tuned communication can lead to many health issues, from gastrointestinal disorders to mental health conditions.
The gut-brain axis plays a pivotal role in managing our body’s response to various digestive functions, from the absorption of nutrients to the expulsion of waste. When this communication system experiences disruptions, it can result in gastrointestinal disorders such as:
- Irritable Bowel Syndrome (IBS): Characterized by chronic abdominal pain, bloating, and altered bowel habits, IBS is a common disorder that’s been closely linked to imbalances in the gut-brain axis. The brain’s increased sensitivity to gut stimuli can lead to heightened pain perception, contributing to IBS symptoms.
- Inflammatory Bowel Disease (IBD): Includes conditions like Crohn’s disease and ulcerative colitis, where parts of the digestive tract become inflamed. Emerging research suggests that disruptions in the gut-brain axis can influence the immune response, exacerbating inflammation and worsening IBD symptoms.
Mental Health and the Gut-Brain Axis
The implications of the gut-brain axis go beyond physical health, impacting mental well-being too. The gut, often called the “second brain,” houses an intricate network of neurons and produces a variety of neurotransmitters, influencing our mood and mental state. Disruptions in this axis have been linked to mental health conditions such as:
- Anxiety: Research indicates a strong correlation between gut health and anxiety disorders. An imbalanced gut microbiome, a potential result of disrupted gut-brain communication, can increase anxiety levels.
- Depression: Imbalances in the gut-brain axis can influence the onset of depression. The gut microbiome plays a role in producing serotonin, the “feel-good” neurotransmitter. Disruptions in this production process could potentially contribute to depressive symptoms.
Gut-Brain Axis on Metabolism and Weight Regulation
The gut microbiome plays a large role in energy balance and metabolism. The bacteria in your gut can affect how you digest foods, influencing the amount of energy you get from your diet and how much fat you store. Some research has shown that an imbalanced gut microbiome can predispose you to obesity and metabolic disorders like type 2 diabetes.
The gut microbiota can influence appetite regulation. They communicate with the brain through hormones, neurotransmitters, and other metabolic products to signal feelings of hunger or satiety. For example, certain gut bacteria produce short-chain fatty acids (SCFAs) like butyrate when they digest dietary fiber. These SCFAs interact with the cells in your gut and can signal your brain to adjust your appetite, potentially contributing to weight management.
Impact of Gut-Brain Axis on Nutrient Absorption
The gut-brain axis and the gut microbiome are essential in nutrient absorption. The bacteria in your gut aid in the digestion of complex carbohydrates, proteins, and fats, breaking them down into components your body can use. Moreover, certain gut bacteria are responsible for synthesizing vitamins like vitamins K and B, which are vital for overall health.
A healthy and diverse gut microbiome can ensure the optimal absorption and use of nutrients from your diet. But an imbalance in the gut microbiome (dysbiosis) can disrupt this process, leading to nutrient deficiencies and related health problems.
Impact on Gut-Brain Immune Function
About 70% of our immune system resides in the gut, reflecting the critical role of the gut in immune response and disease resistance. The gut microbiota can influence the development and function of the immune system, helping protect against pathogens and supporting immune tolerance to avoid harmful overreactions.
A healthy gut microbiome can promote a balanced immune response, while gut microbiome dysbiosis can contribute to inflammatory and autoimmune diseases. The gut-brain axis can also influence immune response indirectly, as stress and emotional factors (mediated through the brain) can affect gut health and, subsequently, immune function.
How to Support Your Gut-Brain Health
- Balanced Diet – Diet plays a crucial role in shaping the gut microbiota and the functioning of the gut-brain axis. A balanced, diverse diet can help maintain a healthy and diverse gut microbiome, which is essential for optimal gut-brain communication. Eating a diet rich in fiber can be beneficial as fiber serves as fuel for healthy gut bacteria. This includes many fruits, vegetables, whole grains, legumes, nuts, and seeds. Fermented foods like yogurt, kefir, sauerkraut, kimchi, and kombucha are also beneficial as they contain probiotics, which can help boost healthy gut bacteria populations. Limiting processed foods and those high in sugar and fat can promote the growth of harmful bacteria and contribute to dysbiosis.
- Regular Exercise – Exercise can have a positive effect on the gut microbiome. Studies have shown that regular physical activity can increase microbial diversity, which is often linked to better health. Additionally, exercise helps manage stress levels and promotes better mood and mental health, indirectly supporting the gut-brain axis, as chronic stress can disrupt the gut balance.
- Adequate Sleep – Good sleep is essential for overall health and affects the gut microbiome. Sleep deprivation or disrupted sleep patterns can lead to an imbalance in the gut microbiota, affecting gut-brain communication. Regular and enough sleep each night can help maintain a healthy gut-brain axis.
- Stress Management – Stress can have a significant impact on gut health. Chronic stress can disrupt the balance of the gut microbiota and negatively affect the gut-brain axis. Implementing stress management techniques, such as mindfulness, meditation, yoga, or other relaxation practices, can help manage stress levels and positively impact gut health.
Contact Us
The gut-brain connection’s influence on our mental and physical health highlights its importance, and a better understanding of this intricate link can enable us to take better care of ourselves. We can actively nourish our gut-brain health with a balanced diet, regular exercise, adequate sleep, and effective stress management. Don’t delay care if you have persistent gut health problems or concerns. Our trusted experts provide quality care with compassion. Reach out to Gastroenterology of Greater Orlando today!