
Managing GERD: Lifestyle and Dietary Tips for Relief
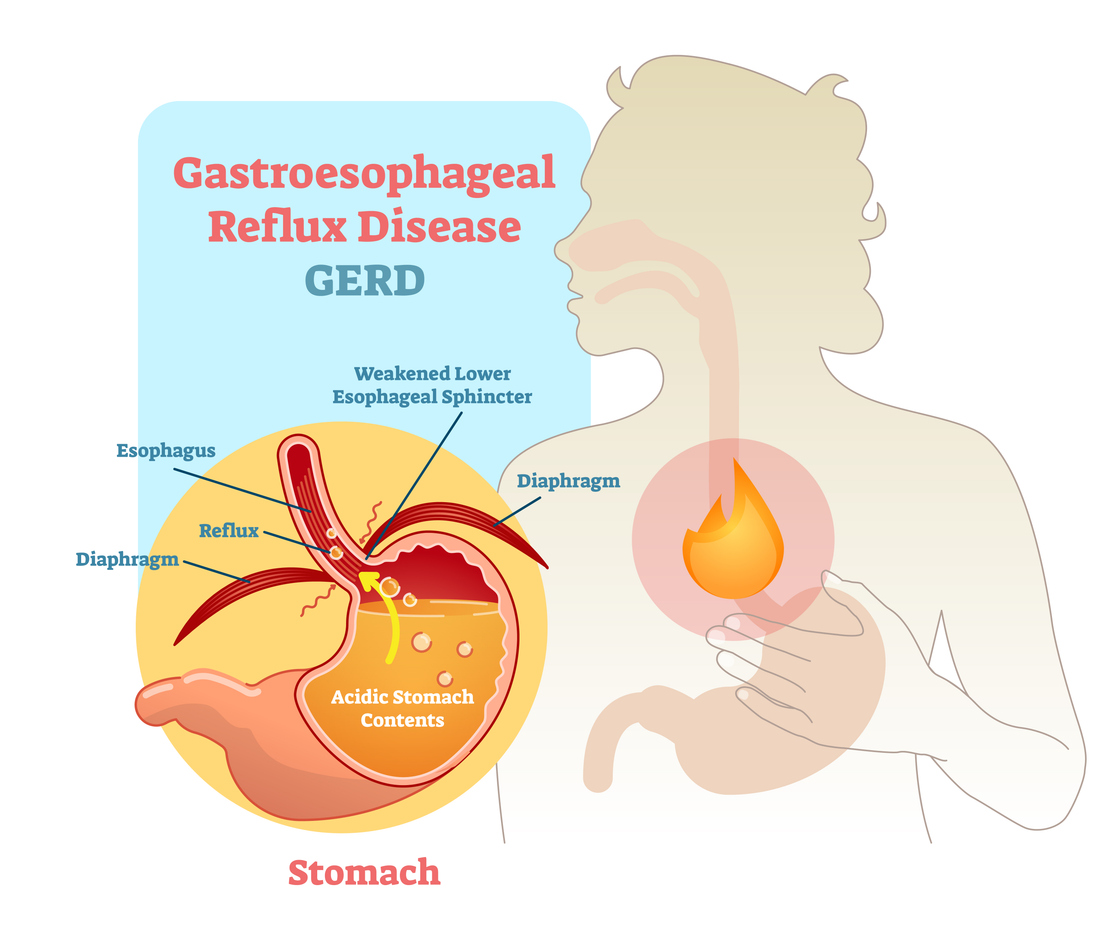
GERD, or gastroesophageal reflux disease, is a chronic issue that occurs when stomach acid flows back into the esophagus. This can lead to symptoms such as heartburn, regurgitation, and discomfort. Acid reflux happens occasionally in many people, but it’s a milder form of the issue. GERD is more severe and lasts longer, so it needs ongoing management.
- Eat Smaller, More Frequent Meals
-
- Problem: Big meals often trigger GERD symptoms. They raise pressure on the lower esophageal sphincter (LES), the valve between the esophagus and stomach. When the LES is under pressure, stomach acid may leak into the esophagus, leading to heartburn and acid reflux.
- Solution: Instead of consuming three large meals daily, try eating smaller, more frequent meals. This can help reduce pressure on the LES and allow your body to digest food more efficiently. Aim to have 5-6 smaller meals throughout the day, spaced out every 3-4 hours.
2. Avoid Trigger Foods and Beverages
-
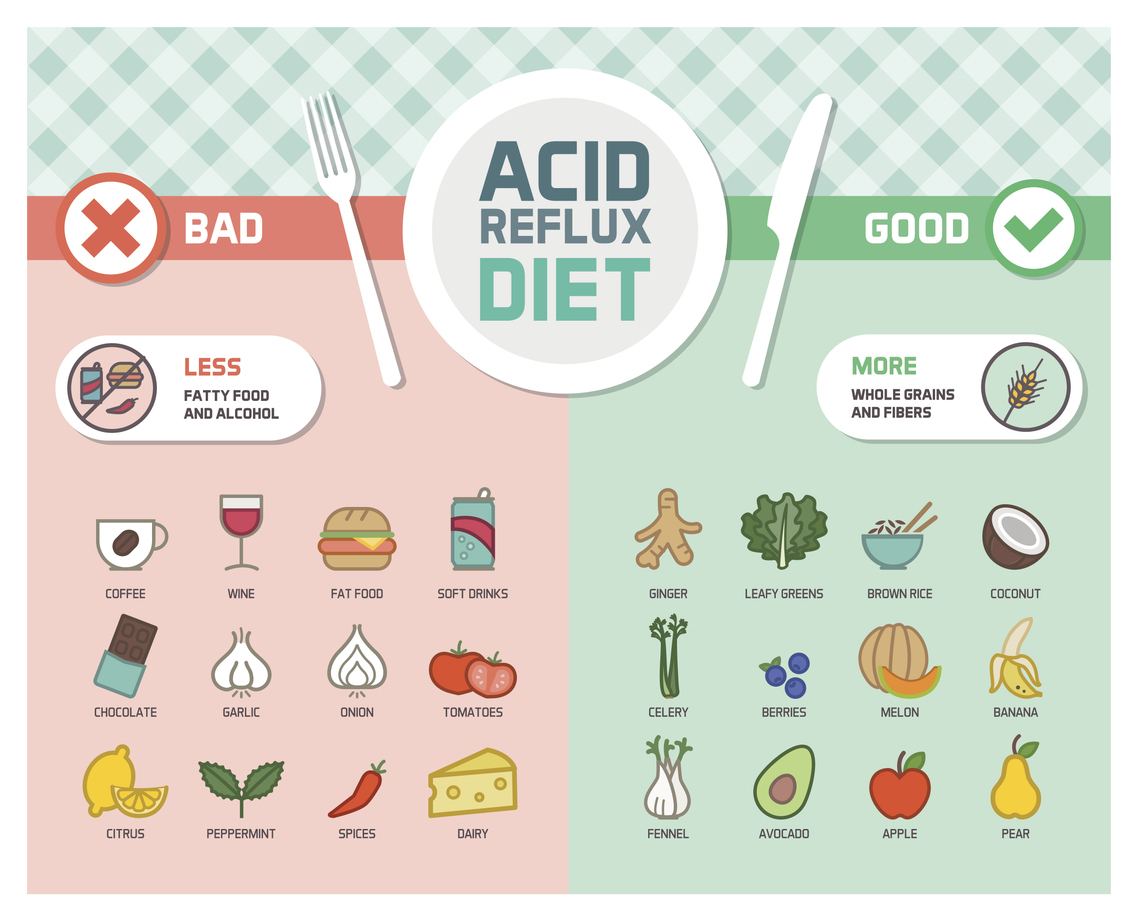
- Problem: Some foods and drinks can relax the LES or boost stomach acid. This can make GERD symptoms worse. Common triggers include: spicy foods, citrus fruits and juices, tomato-based products, chocolate, peppermint, fatty or fried foods, caffeinated beverages, carbonated drinks, and alcohol.
- Solution: Identify the foods that trigger your GERD symptoms and try to eliminate or reduce them in your diet. Keeping a food diary can help you track what causes flare-ups. Avoiding these triggers can reduce your chances of heartburn and other GERD symptoms.
3. Incorporate Alkaline and pH-Balancing Foods
-
- Problem: Some foods can worsen GERD symptoms. Others can help by neutralizing stomach acid and reducing irritation. Alkaline foods, like vegetables, non-citrus fruits, and whole grains, can help manage GERD. They are less likely to cause reflux.
- Solution: Include foods that are more alkaline and pH-balancing in your diet, such as: bananas, oatmeal, green leafy vegetables (spinach, kale), ginger, non-citrus fruits (apples, melons), whole grains (brown rice, quinoa), and nuts and seeds (almonds, flaxseeds). These foods help maintain a balanced pH in the stomach, reducing acid reflux and relieving GERD symptoms.
- Stay Upright After Eating
-
- Problem: Lying down right after eating can cause acid reflux. This happens because it lets stomach contents move up the esophagus more easily. It’s important to give your body time to digest before reclining.
- Solution: Stay upright for at least 2-3 hours after eating. This will prevent acid from moving back into your esophagus and lower the chances of heartburn or regurgitation. If you must rest after a meal, try sitting in a comfortable chair instead of lying flat.
- Elevate the Head of Your Bed
-
- Problem: Many people experience GERD symptoms, such as heartburn or regurgitation, while sleeping. This is because lying flat in bed allows stomach acid to flow back into the esophagus more easily. Elevating the head of your bed can help reduce the frequency of nighttime symptoms.
- Solution: Elevate the head of your bed by 6-8 inches using a wedge pillow or by adjusting the legs of the bed. This will help gravity keep stomach acid where it belongs and reduce nighttime reflux. It’s important to avoid using extra pillows to prop yourself up, as this may increase pressure on your abdomen and worsen symptoms.

6. Maintain a Healthy Weight
-
- Problem: Being overweight or obese increases the risk of GERD, as excess weight can put additional pressure on the abdomen and the LES, leading to acid reflux. Losing weight, even in small amounts, can positively impact GERD symptoms and overall health.
- Solution: If you carry extra weight, try making small changes to your diet and exercise. This can help you reach and keep a healthy weight. Include regular exercise like walking, swimming, or cycling. Also, eat a balanced diet rich in vegetables, lean proteins, and whole grains. If you’re unsure where to begin, talk to your healthcare provider or a nutritionist. They can help you create a weight-loss plan that fits your needs.
- Quit Smoking
-
- Problem: Smoking weakens the LES, making it more likely that stomach acid will flow into the esophagus. Smoking can raise stomach acid production. It also slows the healing of esophageal tissue. If you smoke, quitting can significantly improve your GERD symptoms.
- Solution: Quitting smoking is one of the most effective ways to reduce GERD symptoms. It might take time, but you can beat this habit. Smoking cessation programs, support groups, and nicotine replacement therapies can help you improve your health.
- Practice Stress Management Techniques
-
- Problem: Stress and anxiety can exacerbate GERD symptoms, potentially leading to increased stomach acid production and more frequent reflux episodes. Managing stress through relaxation techniques can help alleviate GERD-related discomfort.
- Solution: Incorporate stress management strategies into your daily routine, such as: deep breathing exercises, yoga, meditation, and progressive muscle relaxation. These techniques can help lower your stress levels and may reduce the frequency of GERD flare-ups. Additionally, getting adequate sleep and finding time for enjoyable activities can support overall well-being and digestive health.
- Limit or Eliminate Alcohol Consumption
-
- Problem: Alcohol is known to relax the LES and increase stomach acid production, which can lead to acid reflux and heartburn. Even moderate drinking can contribute to GERD symptoms, especially if consumed before bed.
- Solution: If you’re prone to GERD, it’s a good idea to limit your alcohol intake or eliminate it entirely. If you choose to drink, do so in moderation and avoid drinking on an empty stomach, as this can increase the likelihood of reflux.
- Consult Your Doctor for Medication Options
-
- Problem: GERD symptoms persist despite lifestyle and dietary changes. If your symptoms continue, additional medical treatment may be necessary to manage the condition.
- Solution: Consult your doctor for medication options. Your doctor may recommend antacids (e.g., Tums, Maalox), H2 blockers (e.g., ranitidine, famotidine), or proton pump inhibitors (PPIs) (e.g., omeprazole, esomeprazole) to reduce stomach acid and provide relief. Be sure to discuss the long-term use of these medications and their potential side effects with your doctor.
Contact Us
Managing GERD often requires a combination of lifestyle and dietary adjustments. These changes can reduce symptoms and improve quality of life. However, everyone is different, and what works for one person may not work for another.
If you have GERD or need a custom treatment plan, contact the experts at Gastroenterology of Greater Orlando. Our team is here to provide the care and guidance you need to manage GERD effectively and live a more comfortable, symptom-free life. Contact us today to schedule a consultation and start your journey toward better digestive health.