Blood In Your Stool Symptoms and What It Means
Your stool often provides significant clues about your general health. Sometimes, the color, texture, size, and shape of this excreted material enables doctors to detect a potential underlying illness.
One alarming sight occasionally seen in stools is blood. In some instances, this results from minor and easily fixable problems. Other times its presence is a symptom of a serious and possibly life-threatening condition.
How Blood Appears in Stool
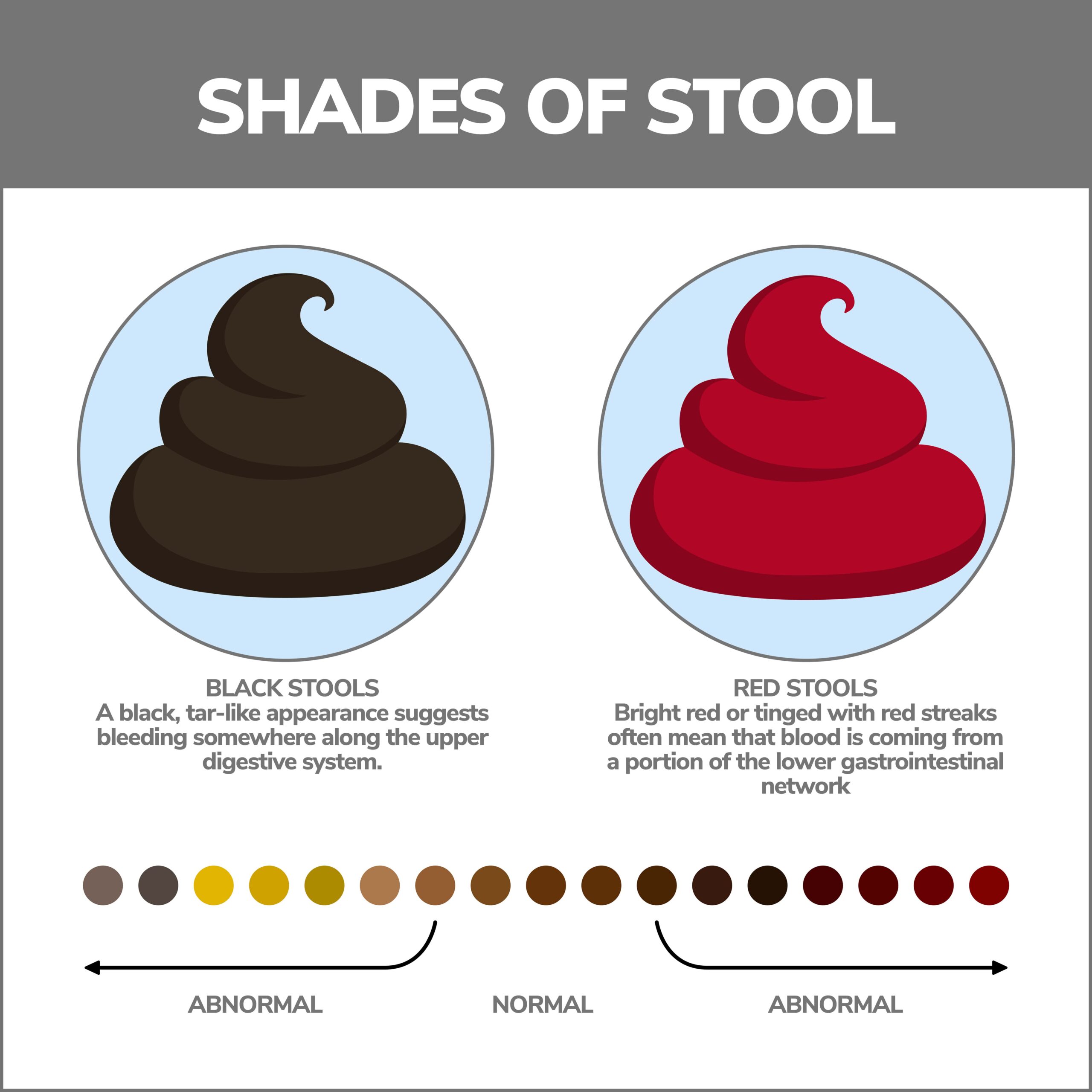
The blood’s coloring typically indicates where along your digestive tract the bleeding originated.
- Black Stools – Fecal material with a black, tar-like appearance suggests bleeding somewhere along the upper digestive system. The Upper GI is made up of the mouth, esophagus, stomach, and higher reaches of the small intestine.
- Red Stools – Stools that appear bright red or tinged with red streaks often mean that blood comes from a part of the lower gastrointestinal network or the Lower GI. Components of the Lower GI include the large intestine (colon), the rectum, and the anus.
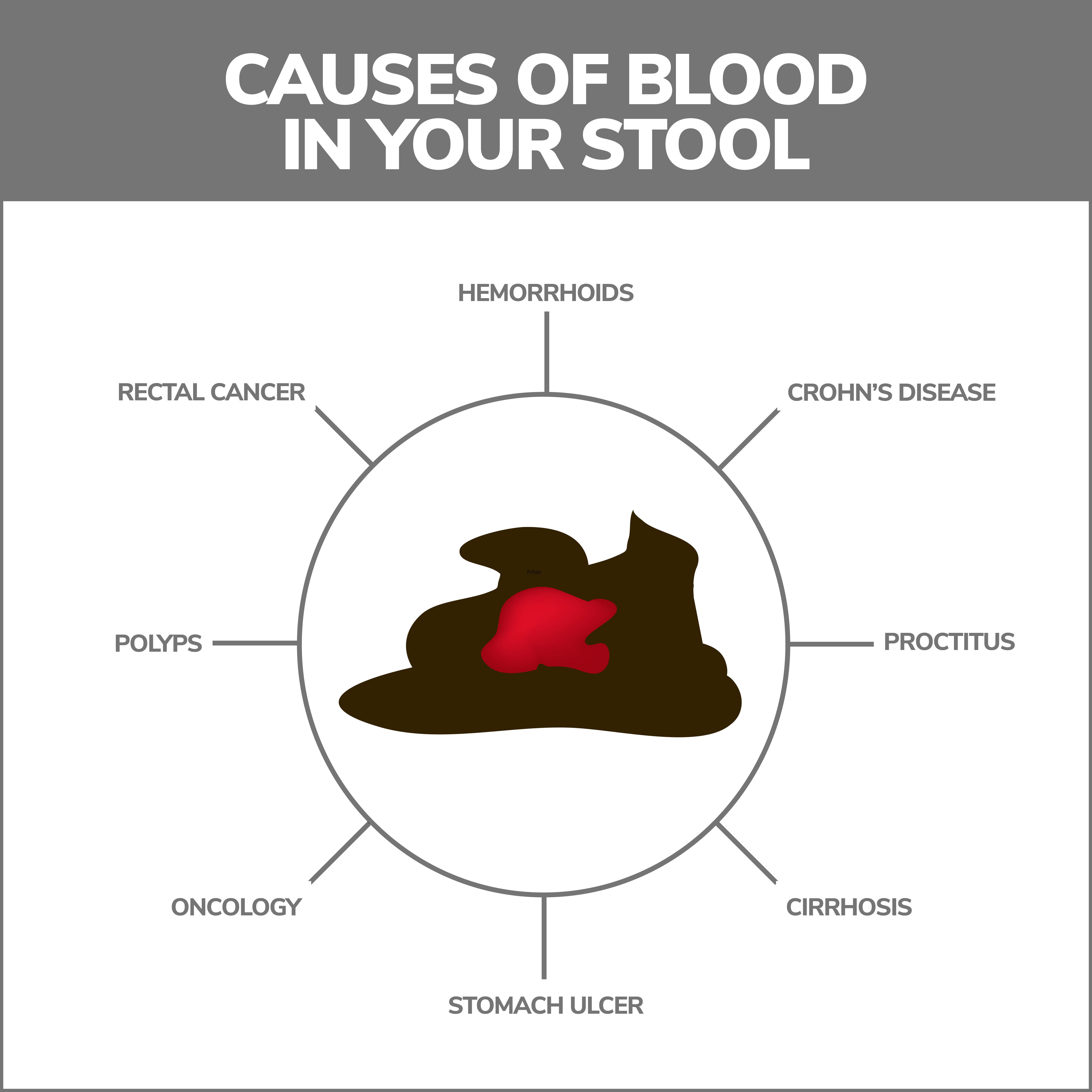
Possible Underlying Causes
It is important to remember that bleeding is a symptom of a more significant underlying problem. Common causes of blood in the stool include:
- Digestive Tract Ulcers – Ulcers are sores developing along the stomach’s lining or the top section of the small intestine (duodenum). Ulcers are caused by inflammation capable of eroding affected tissues. Bleeding may result when the erosion becomes pronounced enough or ulcers are located near blood vessels. Besides blood in the stools, you might also experience symptoms such as decreased appetite, unintentional weight loss, upper abdominal pain, weakness, heartburn, and belching.
- Inflammatory Bowel Disease – The term inflammatory bowel disease, sometimes abbreviated IBD, refers to certain conditions where inflammation develops inside gastrointestinal network components and damages the tissues of those organs. Occasionally, these diseased tissues bleed. The two most common forms of IBD are Crohn’s Disease, which could strike many digestive tract components, and ulcerative colitis, which impacts the colon.
- Diverticulitis – Diverticula are small sacs found in your colon. These features can grow inflamed and ultimately infected, resulting in a condition known as diverticulitis. Aside from bleeding, the condition can produce symptoms such as abdominal pain, gas, and bloating.
- Hemorrhoids – Hemorrhoids are enlarged veins in your rectum and anus. When these blood vessels grow swollen enough, they bleed. Following bowel movements, blood usually appears as streaks of red blood on toilet paper. Blood might also be visible in stools. Hemorrhoids are also commonly accompanied by pain, burning, and itching in the anal region.
- Gastroenteritis – This illness often emerges after you consume spoiled or contaminated food or water. It causes symptoms like diarrhea, nausea, vomiting, and abdominal pain for several days. Severe inflammation brought on by the pathogens may also result in bloody stools.
- Anal Fissures – Anal fissures are small tears developing in your anus’s lining. They often bleed following bowel movements.
- Colon Polyps – These sometimes precancerous growths may cause blood in the stools. In some instances, they do not cause any other symptoms.
- Cancer – Cancer is the most serious of all illnesses, capable of causing bloody stools. Malignancies of any digestive tract component can produce alarming symptoms. Cancer might also precipitate other red-flag symptoms such as unintentional weight loss, severe fatigue, loss of appetite, and vomiting.
- Drugs – Certain medications produce bloody stools. Common culprits are blood thinning agents. Common over-the-counter stomach-soothing preparations might cause black stools. This results from how the medication is broken down inside your body and does not necessarily show that you are experiencing an underlying health issue.
When Should You Visit Your Doctor?
Blood in your stool should always be reported to your doctor immediately. It indicates that something is going on inside your body that requires identification and treatment. Even if the bleeding is light, occasional, or not accompanied by any other symptoms, you should not hesitate to contact your doctor.
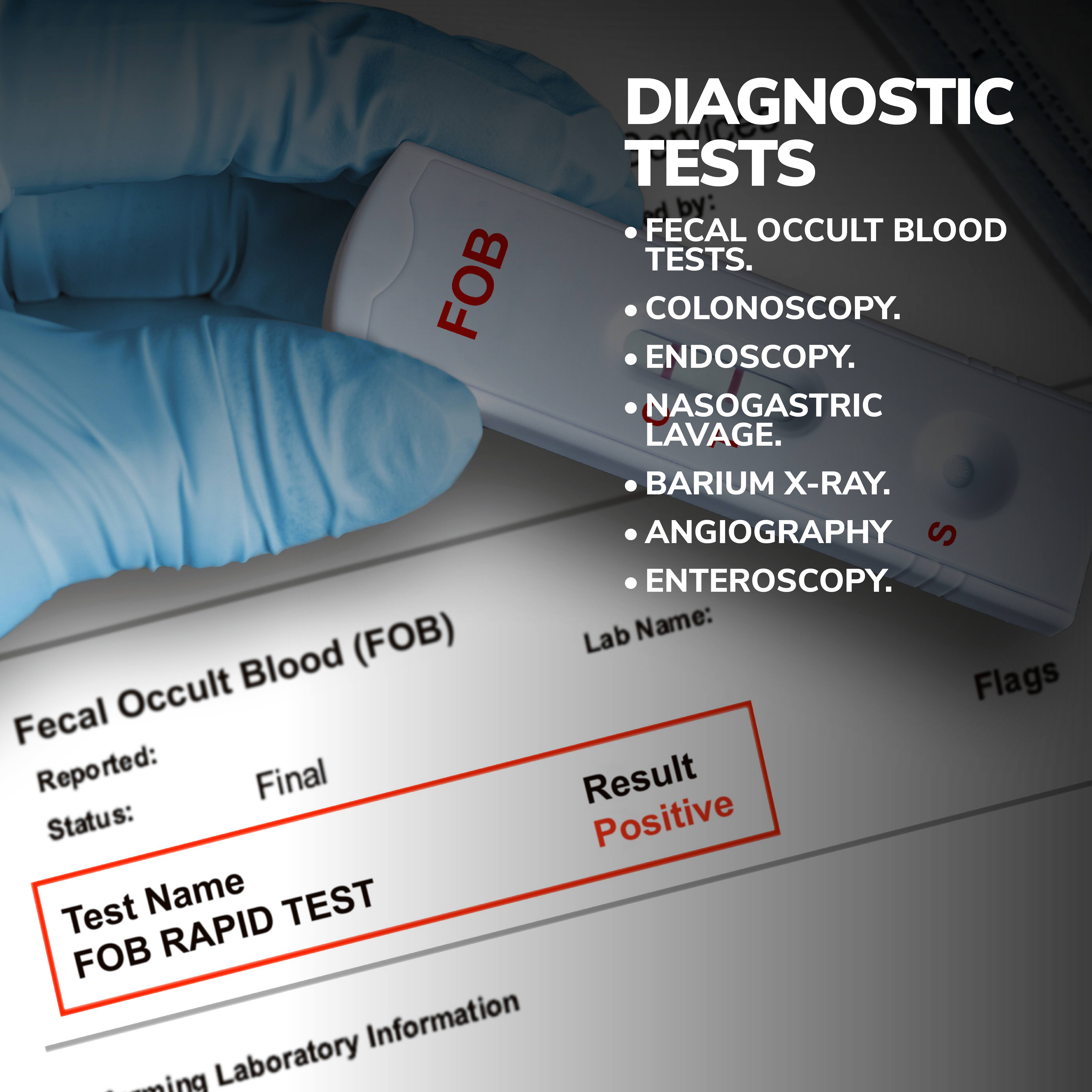
Diagnosing The Underlying Condition
Based on the color of the blood and other symptoms, your doctor could order any number of diagnostic tests, including:
- Fecal occult blood tests.
- Colonoscopy.
- Endoscopy.
- Nasogastric lavage.
- Barium X-Ray.
- Angiography
- Enteroscopy.
If these internal imaging tests do not produce the intended results, your doctor might order exploratory surgery called laparoscopy. During this procedure, surgeons open your abdomen to search for visible irregularities.
How Is Blood in The Stool Treated?
If bleeding needs to be stopped immediately, doctors can administer clot-producing drugs or use surgical tools to stitch or repair affected blood vessels or tissue.
Specific longer-term treatment will hinge on the issue causing the problem. Common treatments include:
- Medications – Antibiotics can eradicate existing bacteria, and inflammation-reducing preparations might produce favorable results in curtailing incidents of IBD.
- Home Care Remedies – If simple, readily fixable causes are to blame, home care methods such as altering your diet, reducing stress, or limiting your indulgence in potentially harmful vices might prove beneficial.
- Surgery – If the problem results from colon polyps or cancer, surgery can be used to remove the diseased tissue.
Recovery
Bleeding can often be controlled enough to prevent immediate or dangerous problems. Recovery from the underlying cause will vary depending on the specific issue, the problem’s severity, your age, overall health, and the form of treatment employed.
Preventing Future Incidents of Bloody Stools
Not every case is preventable. You may lessen your risk by engaging in preventative measures such as:
- Eating Nutritious Foods – Eating natural foods like lean meats, produce, and grain products can reduce the amount of inflammation inside your body.
- Limiting Or Eliminating Potentially Harmful Vices – You are strongly urged to cut back on or completely stop engaging in excessive alcohol intake or cigarette smoking. Alcohol is okay if enjoyed in strict moderation. Doctors recommend not smoking because of its potentially harmful effects on the digestive tract and other bodily regions.
- Staying Hydrated – A simple act like drinking water often improves digestion. A normal-functioning digestive tract produces bowel movements that are easy to pass, which could reduce incidents of anal fissures and hemorrhoids.
- Getting Regular Medical Checkups – Persons with a history of digestive system cancers are urged to get routine screenings. Tests like colonoscopies can detect cancer in its earliest and most curable stages.

Contact Us
If you see blood in your stools, please contact the highly skilled team of well-versed specialists working for Gastroenterology of Greater Orlando. Our practice began more than 15 years ago and has emerged as one of the leading gastroenterology practices in central Florida. We perform a host of diagnostic procedures using state-of-the-art equipment in a friendly, comfortable, and inviting atmosphere where patient care is always a top priority. Contact us today!