
Navigating Necrotizing Pancreatitis: Causes, Symptoms, and Treatment Options
Necrotizing pancreatitis is a severe and potentially life-threatening form of pancreatic inflammation that requires prompt medical attention. Characterized by inflammation of the pancreas, this condition can lead to tissue death (necrosis) within the pancreas and surrounding tissues and organs, resulting in the demise and deterioration of pancreatic tissue and its adjacent structures.
What Causes Necrotizing Pancreatitis?
The primary causes of necrotizing pancreatitis are similar to those of acute pancreatitis, but the severity of the condition is often more pronounced. Some of the most common causes of necrotizing pancreatitis include:
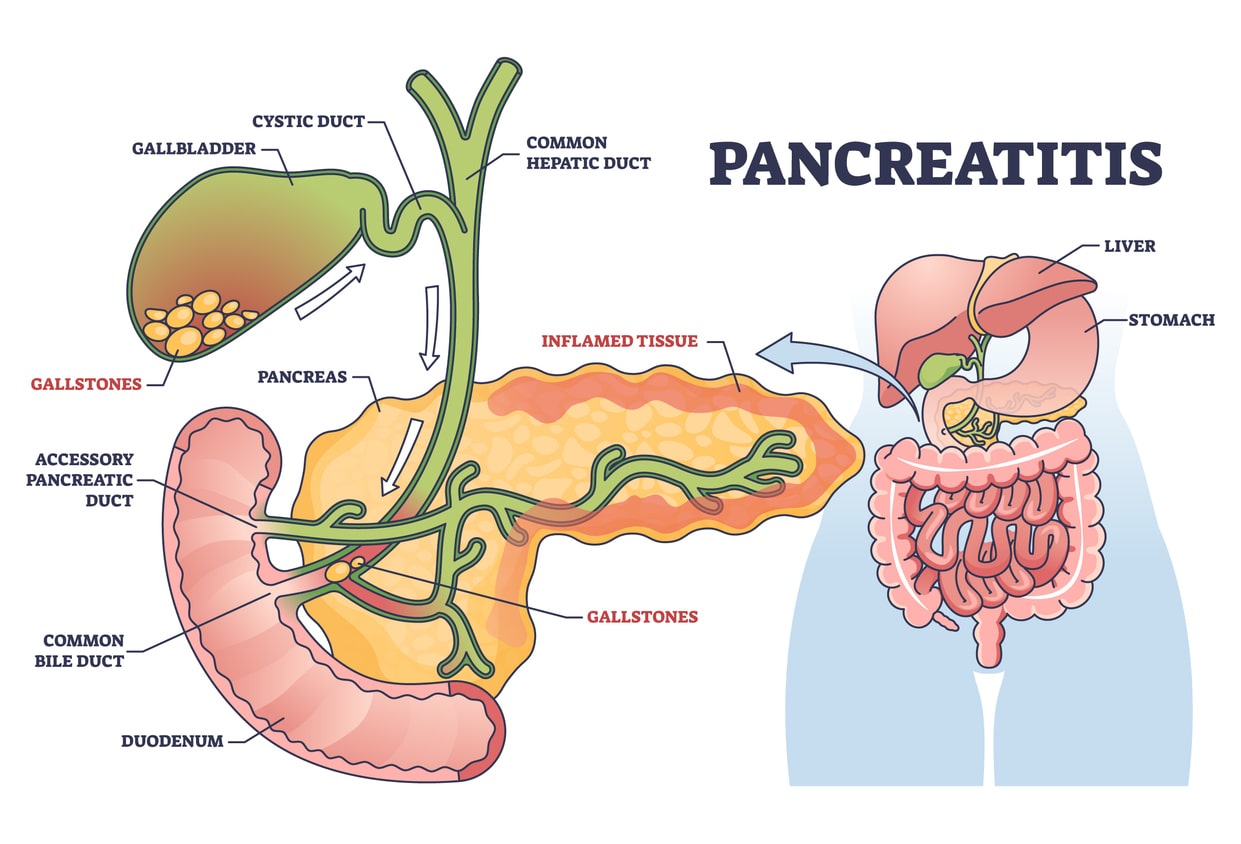
- Gallstones: Gallstones are the leading cause of necrotizing pancreatitis, accounting for up to 80% of cases. When gallstones block the bile or pancreatic duct, they can trigger the release of digestive enzymes, leading to pancreatic inflammation and necrosis.
- Excessive Alcohol Consumption: Chronic alcohol abuse is another significant risk factor for necrotizing pancreatitis, as it can cause inflammation and damage to the pancreas.
- Medications: Specific medications, such as certain antibiotics, diuretics, and antidepressants, have been associated with an increased risk of developing necrotizing pancreatitis.
- Trauma: Physical trauma to the abdomen, such as from a car accident or a fall, can also lead to the development of necrotizing pancreatitis.
- Metabolic Disorders: Conditions like hypertriglyceridemia (high levels of triglycerides in the blood) and hypercalcemia (high levels of calcium in the blood) can increase the risk of necrotizing pancreatitis.
Understanding the underlying causes of necrotizing pancreatitis is crucial for developing an effective treatment plan and preventing the recurrence of the condition.
Symptoms of Necrotizing Pancreatitis
The symptoms of necrotizing pancreatitis can be severe and often develop rapidly. Some of the most common symptoms include:
- Severe Abdominal Pain: Often radiating to the back, this is a hallmark symptom of necrotizing pancreatitis and is typically intense and persistent.
- Nausea and Vomiting: Patients with necrotizing pancreatitis often experience nausea and vomiting due to the inflammation and irritation of the gastrointestinal tract.
- Fever and Chills: Inflammatory processes associated with necrotizing pancreatitis can lead to fever and chills as the body’s immune system responds to infection or tissue damage.
- Abdominal Tenderness or Rigidity: The abdomen may feel tender to the touch or become rigid due to inflammation and tissue damage
- Jaundice: Yellowing of the skin and eyes (jaundice) may occur if the bile duct becomes obstructed due to pancreatitis-related inflammation.
Diagnosing Necrotizing Pancreatitis
Diagnosing necrotizing pancreatitis requires a comprehensive assessment by your physician, often involving a combination of clinical evaluation, laboratory tests, and imaging studies. Initial evaluation typically includes a thorough medical history and physical examination to assess symptoms such as severe abdominal pain, fever, and gastrointestinal distress. Blood tests may be conducted to evaluate pancreatic enzyme activity and assess for inflammation. Imaging tests such as computed tomography (CT) scans or magnetic resonance imaging (MRI) are instrumental in visualizing pancreatic tissue and detecting signs of necrosis. In some cases, endoscopic retrograde cholangiopancreatography (ERCP) or ultrasound-guided fine needle aspiration may be performed to obtain tissue samples for further analysis. Prompt and accurate diagnosis of necrotizing pancreatitis is essential for initiating appropriate treatment and managing potential complications associated with this severe condition.
Complications Associated with Necrotizing Pancreatitis
Necrotizing pancreatitis can lead to a range of severe complications, which can significantly impact your health and well-being. Some of the most common complications include:
- Organ Failure: Necrotizing pancreatitis can cause the failure of vital organs, such as the kidneys, lungs, and cardiovascular system.
- Infection: The necrotic (dead) tissue in the pancreas can become infected, leading to the development of pancreatic abscesses or infected necrosis, which can be life-threatening.
- Bleeding: Necrotizing pancreatitis can cause damage to blood vessels, leading to internal bleeding and the formation of pseudoaneurysms (weakened blood vessel walls).
- Fluid Collections and Abscesses: The destruction of pancreatic tissue can result in the accumulation of fluid and the formation of abscesses (collection of pus), which can further complicate the condition.
- Diabetes: Severe and extensive pancreatic necrosis can lead to the development of diabetes due to the destruction of insulin-producing cells.
Recognizing and managing these complications is crucial for improving the outcomes and reducing the risk of mortality in individuals with necrotizing pancreatitis.

Treatment Options
Treating necrotizing pancreatitis typically involves a multifaceted approach, with the primary goal of managing the underlying cause, preventing complications, and supporting the patient’s overall health. Popular treatment options include:
Non-Surgical Interventions:
- IV Fluids: In managing necrotizing pancreatitis, intravenous (IV) fluids play a vital role by addressing fluid loss, ensuring hydration, and restoring electrolyte balance.
- Antibiotics: Antibiotics are often prescribed to prevent or treat infections, which are common complications of necrotizing pancreatitis.
- Pain Management: Adequate pain management may involve using nonsteroidal anti-inflammatory drugs (NSAIDs) or nerve block procedures to alleviate discomfort.
Surgical Interventions:
- Necrosectomy: This procedure involves removing necrotic (dead) pancreatic tissue to prevent the spread of infection and further complications.
- Debridement: This involves the removal of damaged and infected tissue to promote healing and prevent the spread of infection.
- Pancreatic Resection: In severe cases, a portion of the pancreas may need to be removed (partial pancreatectomy), or the entire pancreas may need to be removed (total pancreatectomy).
Prevention Strategies
While some risk factors for necrotizing pancreatitis, such as genetic predisposition or certain medical conditions, are not easily modifiable, there are steps you can take to reduce your risk:
- Maintain a Healthy Lifestyle: Limit your alcohol consumption, maintain a healthy weight, and follow a balanced, nutrient-rich diet to support your overall health and reduce the risk of pancreatitis.
- Manage Underlying Medical Conditions: If you have conditions like gallstones, hypertriglyceridemia, or hypercalcemia, work closely with your physician to manage these conditions and reduce your risk of developing necrotizing pancreatitis.
- Seek Prompt Medical Attention: If you experience symptoms of pancreatitis, such as severe abdominal pain, nausea, or vomiting, seek medical attention immediately to prevent the condition from progressing.
By taking proactive steps to maintain your health and address any underlying risk factors, you can help reduce your risk of developing necrotizing pancreatitis and its associated complications.
Contact Us
Necrotizing pancreatitis is a severe and potentially life-threatening form of pancreatic inflammation that requires prompt medical attention. Understanding its causes, symptoms, and treatment options empowers you to take proactive steps in preventing and managing this condition effectively. Timely medical intervention is paramount upon experiencing any pancreatitis-related symptoms, making it crucial to seek medical attention immediately.
For comprehensive care tailored to a wide range of gastrointestinal concerns, contact Gastroenterology of Greater Orlando today, where specialized expertise and individualized treatment strategies will help you manage your necrotizing pancreatitis.