Hemorrhoids: Everything to Know
Hemorrhoids (also known as piles) are swollen, inflamed veins in your lower rectum and anus, similar to varicose veins. Internal hemorrhoids develop in the lower rectum, and external hemorrhoids develop under the skin surrounding the anus. They can cause itching, bleeding, and pain and can usually be treated with home remedies. Sometimes they need medical intervention. About 50% of adults experience some type of hemorrhoid symptoms by age 50.
What Causes Hemorrhoids?
Hemorrhoids are caused by excessive pressure on your anus’ veins. Causes and risk factors include:
- Sitting on the toilet for a long time.
- Straining during a bowel movement.
- Having anal sex.
- Having chronic diarrhea or constipation.
- Being obese.
- Having a family history of hemorrhoids.
- Straining to lift heavy objects.
- Being over 50 years old.
- Eating a low-fiber diet.
- Being pregnant.
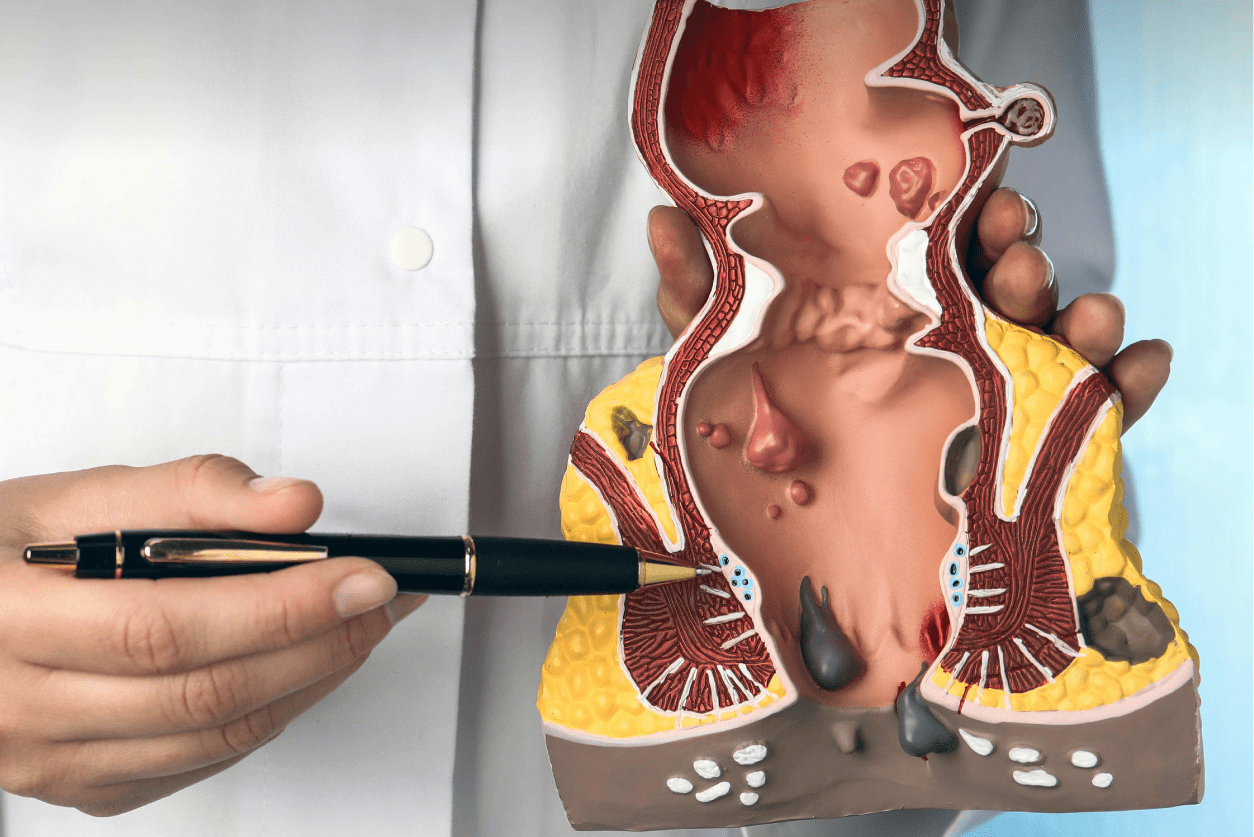
What Are the Types of Hemorrhoids?
There are four types of hemorrhoids:
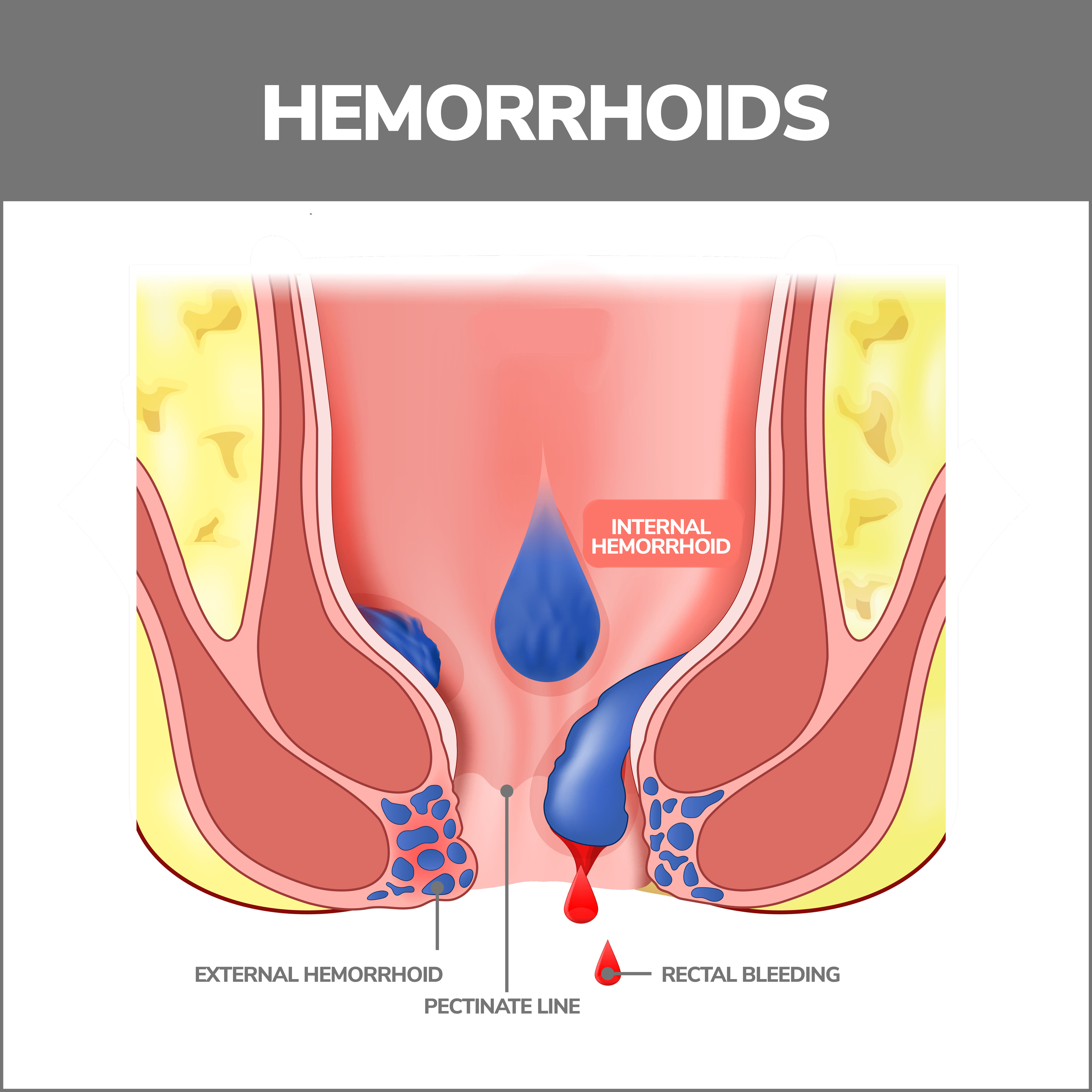
1. Internal Hemorrhoids
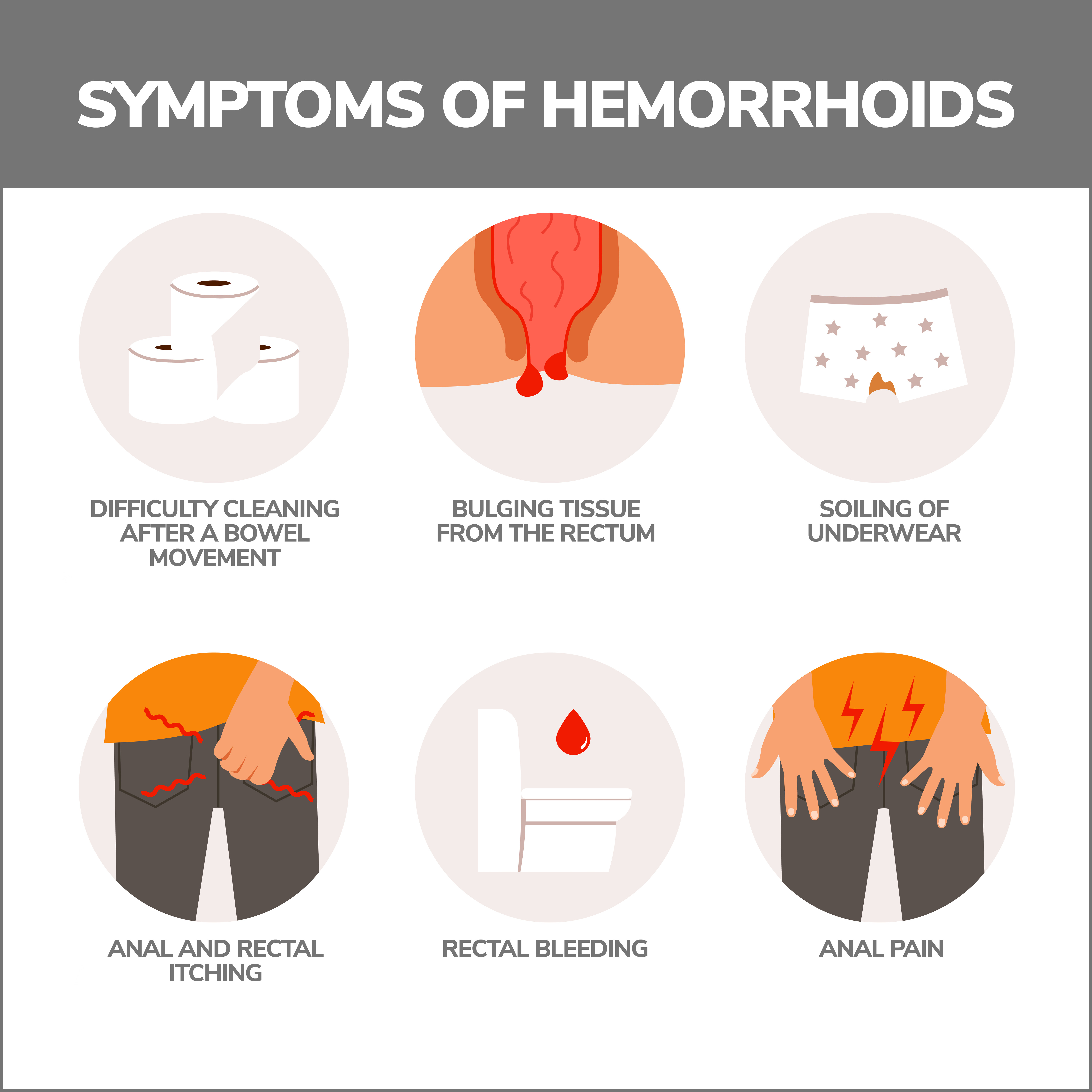
Internal hemorrhoids are bumps that lie far inside your rectum. Few pain-sensing nerves are in this area, so you aren’t usually aware of them. But irritation or straining when you pass a bowel movement can:
- Cause painless bleeding that leaves bright red blood on toilet paper after you wipe or in the toilet bowl.
- Cause a hemorrhoid to prolapse (protrude through the anus’ opening). This can create irritation and pain, but they can usually be pushed back in. Seriously prolapsed hemorrhoids remain protruding from the anus.
2. External Hemorrhoids
These hemorrhoids are small lumps in the skin surrounding your anus. There are many pain-sensing nerves in this area. Symptoms of external hemorrhoids included:
- Pain.
- Itching.
- Swelling.
- Bleeding.
3. Thrombosed Hemorrhoids
Thrombosed hemorrhoids are hemorrhoids in which pooled blood has formed a clot. Symptoms of thrombosed hemorrhoid include:
- Intense pain.
- Itching.
- Bleeding.
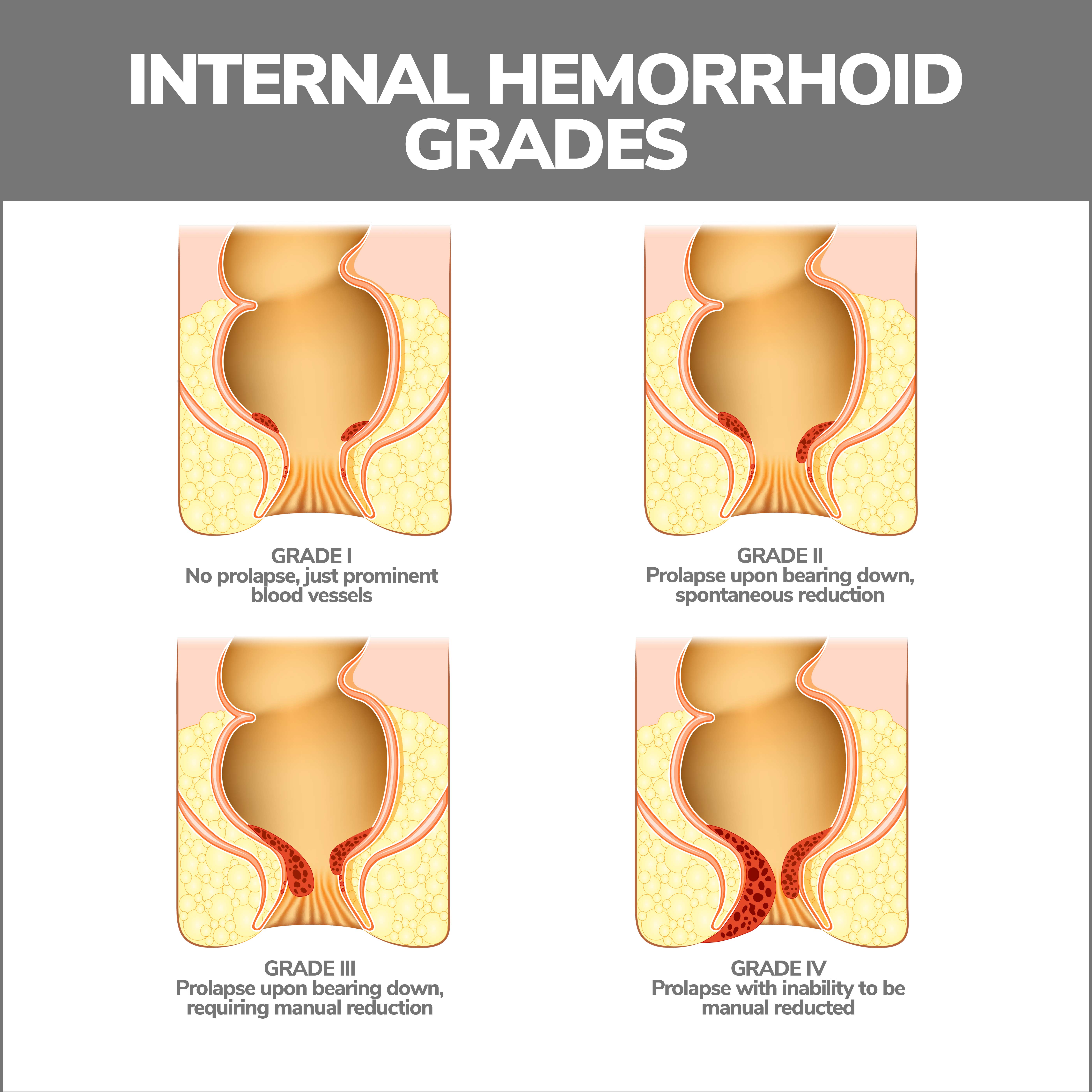
4. Prolapsed Hemorrhoids
A prolapsed hemorrhoid happens when internal hemorrhoids swell and protrude from your anus. Grades are assigned to these hemorrhoids based on how far they stick out:
- Grade One – A Grade One hemorrhoid isn’t prolapsed.
- Grade Two – A Grade Two hemorrhoid is prolapsed but will retract by itself. It may only prolapse under pressure, such as straining to pass a bowel movement but will return to its regular position afterward.
- Grade Three – A Grade Three hemorrhoid is prolapsed, and you need to push it back in. This type of hemorrhoid might need treatment, so it doesn’t hurt or become infected.
- Grade Four – A Grade Four hemorrhoid is prolapsed, and you can’t push it in without pain. These need to be treated to relieve pain and prevent additional complications.
How to Treat Hemorrhoids
You can treat hemorrhoids at home in many ways:
- Soak your hemorrhoids in a sitz bath. A sitz bath is a warm, shallow bath that covers the buttocks and hips and relieves hemorrhoidal pain and itching. Soak in it for 10 to 20 minutes a day. You can use a regular bathtub or a small plastic tub that fits over your toilet seat.
- Use an ice pack. Placing a small ice pack against the anal region for several minutes can help with swelling and pain.
- Use witch hazel wipes. Witch hazel wipes, such as Tucks, can soothe pain and itching.
Other forms of remedies include:
- Over-the-counter hemorrhoid creams containing lidocaine or hydrocortisone can temporarily relieve hemorrhoid pain and itching.
- Nonsteroidal anti-inflammatory medications (NSAIDs) like aspirin, Anvil/Motrin (ibuprofen) and Aleve (naproxen).
- Use toilet paper containing lotion or flushable wet wipes, and pat the area, rather than rubbing.
You may have more than one type of hemorrhoid at a time. Hemorrhoids can be extremely uncomfortable or painful, but they’re not life-threatening.
What Can be Done if Home Remedies Don’t Work?
If these treatments don’t work, or your symptoms get worse, your doctor may do a:
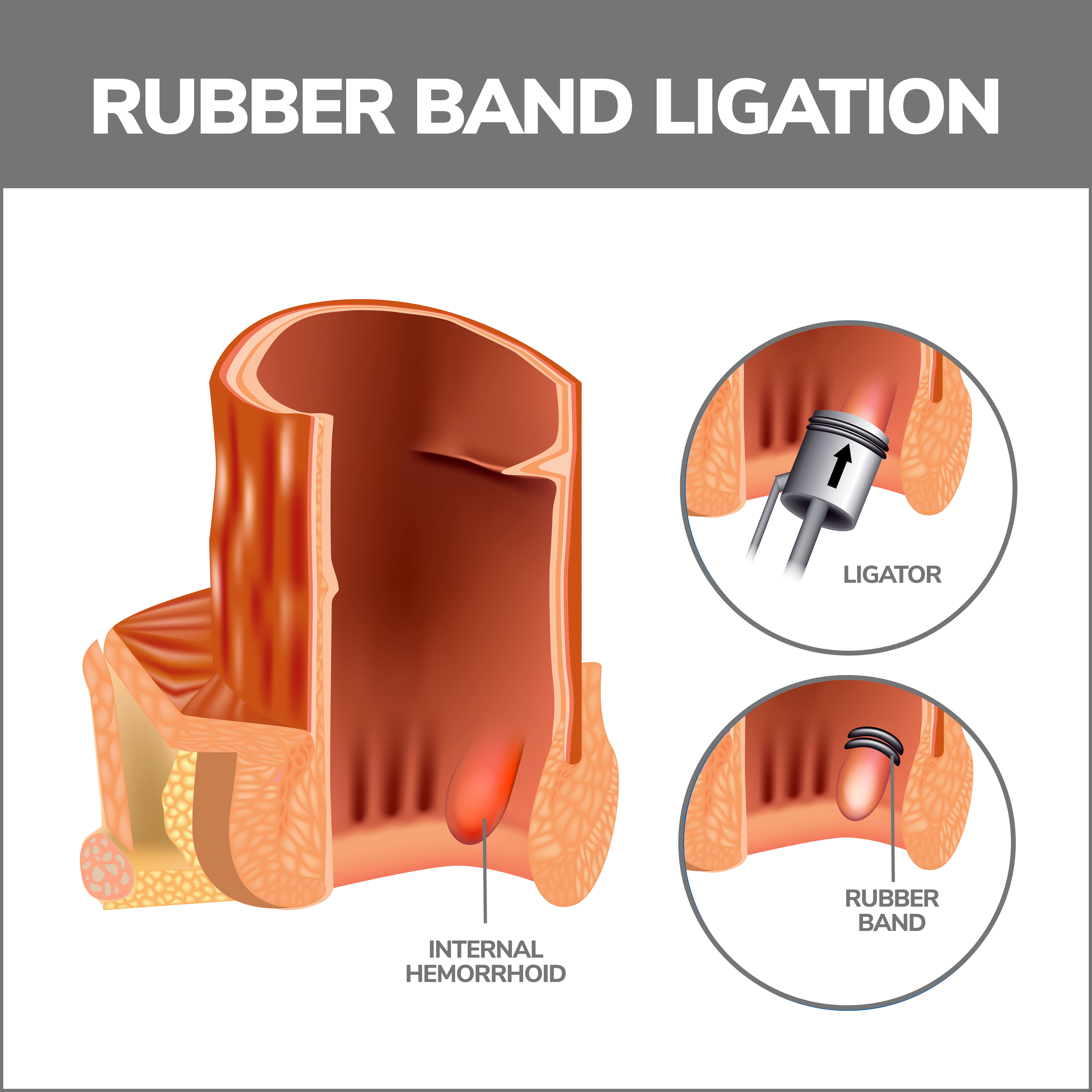
- Rubber Band Ligation – This procedure wraps a small rubber band around the hemorrhoid’s base. This cuts off the vein’s blood supply. It usually takes two to four procedures, performed six to eight weeks apart, to completely remove the hemorrhoid.
- Electrocoagulation – An electrical current stops blood flow to the hemorrhoid during electrocoagulation.
- Infrared Coagulation – A probe inserted into the rectum emits heat that eliminates the hemorrhoid.
- Sclerotherapy – During sclerotherapy, a chemical is injected into the swollen vein that destroys its tissue.
- Hemorrhoidectomy – If rubber band ligation was unsuccessful, or you have large protruding hemorrhoids, hemorrhoidectomy surgery may be necessary.
- An incision is made in the hemorrhoid’s internal and external tissue, and the problematic blood vessels are removed. The procedure has a 95% success rate.
- Stapled Hemorrhoidopexy – Stapled hemorrhoidopexy surgery treats prolapsed or bleeding internal hemorrhoids. The surgeon performing the procedure staples the hemorrhoids back where they belong.
When Should I Call My Doctor?
Call your doctor if you’re experiencing these symptoms:
- Fever and chills.
- Chronic constipation or diarrhea.
- Abdominal pain.
- Nausea and vomiting.
- Severe rectal pain and bleeding.
How to Prevent Hemorrhoids
The best hemorrhoid prevention is keeping your bowel movements soft. You can do this by eating high-fiber foods. Good fiber sources include:
- Brown rice.
- Oatmeal.
- Whole-grain foods.
- Legumes.
- Nuts and seeds.
- Raspberries.
- Apples.
- Pears.
- Broccoli.
Fiber helps bulk up the intestines, which softens bowel movements and makes them easier to pass.
Other preventions include:
- Drinking plenty of water – Aim for six to eight glasses a day.
- Take fiber supplements – Over-the-counter fiber supplements such as Citrucel or Metamucil can improve your hemorrhoid symptoms.
- Don’t strain when you go to the bathroom – When you strain while having a bowel movement, this puts excessive pressure on the lower rectum’s veins.
- Don’t sit too long on the toilet – Sitting too long on the toilet can increase the force on your anus’ veins.
- Exercise – Exercise keeps your bowels moving.
- Go to the bathroom when the urge strikes – The longer you wait, the drier your stool will become and the harder it will be to pass.
Are Hemorrhoids and Anal Fissures the Same Thing?
No. They may have similar symptoms, but they are different. An anal fissure is a small tear or rupture in the thin, moist tissue that lines the anus, while swollen veins cause hemorrhoids.
Anorectal abscesses may also be mistaken for hemorrhoids. These are collections of pus under the skin of the rectum and anus. Anal warts, a type of genital warts, can resemble and feel like a hemorrhoid.
How Are Hemorrhoids Diagnosed?
After giving you a physical exam, your doctor may give you a:
- Digital rectal exam – During this exam, your provider will insert a lubricated, gloved finger into your rectum to feel for anything abnormal such as swollen veins or growths.
- Anoscopy – Your doctor uses a small, tubular instrument called an anoscope to see the inside of your anus.
- Sigmoidoscopy – During a sigmoidoscopy, your doctor uses a sigmoidoscope (a lighted tube with a camera) to observe the last two feet of your colon. Tissue samples can also be removed during a sigmoidoscopy.
- Colonoscopy – If you have rectal bleeding or blood in your feces, a colonoscopy may be done to rule out other potential causes of bleeding, such as colorectal cancer or anal cancer. During this procedure, your doctor looks at your entire colon through a long, thin tube and can also take tissue samples.
Hemorrhoid Complications
Rarely, hemorrhoids can lead to:
- Anemia – If you have a hemorrhoid that lasts a long time and bleeds excessively, you might lose too much blood.
- Infection of an external hemorrhoid.
- Blood clots.
- Skin tags – When a thrombosed hemorrhoid’s clot dissolves, the leftover skin could get irritated.
- Strangulated hemorrhoid.
Sometimes muscles obstruct blood flow to a prolapsed hemorrhoid. This can be extremely painful and need surgery.
Contact Us
Please contact us if you have been diagnosed with hemorrhoids or are experiencing any of the symptoms. Our practice began more than 15 years ago and has emerged as one of the leading gastroenterology practices in central Florida. We perform a host of diagnostic procedures using state-of-the-art equipment in a friendly, comfortable, and inviting atmosphere where patient care is always a top priority. Contact us today!