Crohn’s vs. Colitis: Understanding Symptoms, Causes, and Treatment for IBD
Inflammatory bowel disease (IBD) is an umbrella term for two chronic conditions—Crohn’s disease and ulcerative colitis—that cause ongoing inflammation in the digestive tract. While both share many similarities, they affect the gut in slightly different ways. Living with IBD can be challenging, as symptoms often flare unexpectedly and disrupt daily routines. But with the right treatment and support, most people can manage symptoms, reduce flare-ups, and protect their long-term digestive health. In this comprehensive guide, we’ll explore what Crohn’s and colitis are, the symptoms to watch for, and the treatment options available so you can take control of your digestive health.
What Is Crohn’s Disease?
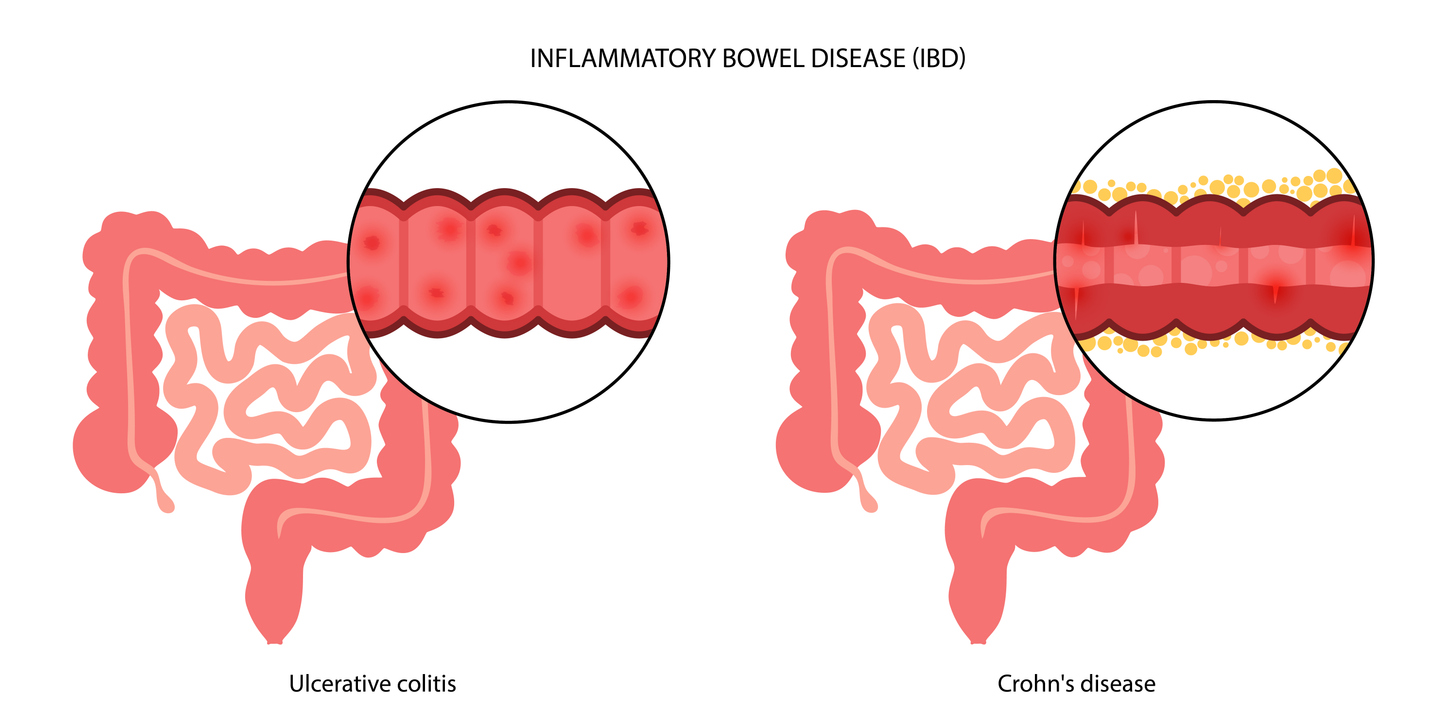
Crohn’s disease is a type of IBD that can affect any part of the gastrointestinal (GI) tract, from the mouth to the anus, though it most commonly impacts the small intestine and the beginning of the colon. The inflammation in Crohn’s disease often occurs in patches, leaving healthy areas between inflamed sections, and can spread deep into the layers of the bowel wall.
Key Characteristics of Crohn’s Disease:
- Affects any part of the GI tract, but commonly the small intestine and colon
- Inflammation often occurs in patches
- Can penetrate multiple layers of the intestinal wall
- May lead to complications such as strictures, fistulas, and abscesses
What Is Ulcerative Colitis?
Ulcerative colitis, the other main type of IBD, primarily affects the large intestine (colon) and rectum. Unlike Crohn’s disease, the inflammation in colitis is continuous, starting in the rectum and extending upward through the colon. It only affects the innermost lining of the colon, rather than penetrating deeper layers.
Key Characteristics of Ulcerative Colitis:
- Affects only the colon and rectum
- Inflammation is continuous rather than patchy
- Limited to the innermost lining of the colon
- Can increase the risk of colorectal cancer if left untreated
Shared Symptoms of Crohn’s and Colitis
Crohn’s disease and ulcerative colitis share many overlapping symptoms, which is why they are grouped together as IBD. However, symptom severity and frequency can vary greatly from person to person. Common symptoms of IBD include the following:
- Abdominal Pain and Cramping: Often caused by inflammation or bowel spasms, pain can range from mild discomfort to severe cramping and is one of the most common signs of IBD.
- Chronic Diarrhea: Frequent, loose stools are a hallmark of IBD. Episodes may be urgent and sometimes include blood or mucus, which can lead to dehydration.
- Fatigue: Ongoing tiredness often stems from inflammation, poor nutrient absorption, or anemia, and can make it difficult to maintain daily energy levels.
- Weight Loss: Unintentional weight loss is common due to reduced appetite, malabsorption, or persistent diarrhea, and may lead to malnutrition over time.
- Rectal Bleeding: More common with ulcerative colitis but also possible with Crohn’s disease, rectal bleeding may appear as blood in the stool or on toilet paper.
- Fever: Low-grade fevers may occur during flares, signaling inflammation or sometimes infection that requires medical attention.
Differences Between Crohn’s and Colitis
Although Crohn’s disease and ulcerative colitis are both forms of IBD, they differ in how and where they cause damage:
- Location: Crohn’s may involve the entire GI tract, while ulcerative colitis is limited to the colon and rectum.
- Inflammation Pattern: Crohn’s appears in patches, while ulcerative colitis spreads continuously.
- Depth of Inflammation: Crohn’s penetrates multiple layers of the bowel wall, while ulcerative colitis affects only the inner lining.
- Complications: Crohn’s is more likely to cause fistulas, strictures, or abscesses, whereas ulcerative colitis increases the long-term risk of colon cancer.
- Surgical Impact: In Crohn’s, surgery can remove damaged sections, but the disease may recur elsewhere. In ulcerative colitis, removing the colon can often cure the condition.
- Symptoms: Crohn’s is more likely to cause pain and malabsorption, while ulcerative colitis more often causes bloody diarrhea and urgency.

Potential Complications
Ignoring symptoms or delaying treatment can increase the risk of serious complications with both Crohn’s and colitis.
Crohn’s Disease Complications:
- Strictures: Narrowing of the intestine due to scarring
- Fistulas: Abnormal tunnels connecting different parts of the bowel or other organs
- Malnutrition: From poor absorption of nutrients
- Abscesses: Pockets of infection in the abdominal wall or intestines
Ulcerative Colitis Complications:
- Severe Bleeding: From ulcerations in the colon
- Toxic Megacolon: A rare but life-threatening widening of the colon
- Perforated Colon: A hole in the colon wall caused by severe inflammation
- Increased Colorectal Cancer Risk: Especially in cases of long-term inflammation
Causes and Risk Factors
The exact cause of Crohn’s disease and ulcerative colitis is not fully understood, but several factors are believed to contribute to their development. Genetics can play a role, as individuals with a family history of inflammatory bowel disease (IBD) are at higher risk. An overactive immune response may also trigger inflammation in the gastrointestinal (GI) tract, causing the body to attack its own tissues. Environmental factors, such as diet, stress, and smoking, can influence disease onset and severity, while certain medications may increase susceptibility. Age, ethnicity, and geographic location also appear to impact risk, with Crohn’s and ulcerative colitis more commonly diagnosed in young adults and individuals of Northern European descent. Understanding these causes and risk factors helps gastroenterologists identify at-risk patients and tailor prevention and management strategies.
Diagnosing Crohn’s and Colitis
Diagnosing Crohn’s disease and ulcerative colitis involves a combination of medical history, physical examination, and specialized tests to evaluate the gastrointestinal (GI) tract. Doctors review symptoms like abdominal pain, diarrhea, rectal bleeding, and fatigue, and may order blood tests to check for inflammation or anemia, as well as stool tests to rule out infections. Imaging studies, such as magnetic resonance imaging (MRI) or computed tomography (CT) scans, can detect inflammation or structural changes in the intestines. Endoscopic procedures, including colonoscopy or upper endoscopy, allow direct visualization of the bowel and enable biopsies for further analysis. This thorough approach helps distinguish between Crohn’s disease and ulcerative colitis, guide treatment, and monitor disease progression.
Treatment Options for IBD
While there is currently no cure for Crohn’s or ulcerative colitis, treatments focus on reducing inflammation, controlling symptoms, and preventing flare-ups.
- Medications: Medicines can help reduce inflammation and control flare-ups when symptoms become more severe.
- Immune System Support: Certain treatments help calm an overactive immune response that can trigger inflammation in the gut.
- Targeted Therapies: Advanced medications focus on specific parts of the immune system for more serious cases.
- Diet and Nutrition: Adjusting your diet or adding supplements can help manage symptoms and prevent nutrient deficiencies.
- Surgery: In some situations, surgery may be needed to fix complications or remove damaged sections of the intestines.
Contact Us
Crohn’s and colitis can be unpredictable, but you don’t have to face them alone. At Gastroenterology of Greater Orlando, our specialists provide expert evaluations, advanced diagnostic tools, and personalized treatment plans to help you manage symptoms and safeguard your digestive health. Whether you’re newly diagnosed or struggling with ongoing flares, we’re here to support you every step of the way. Don’t wait to get the care you deserve—schedule your appointment with Gastroenterology of Greater Orlando today and take the first step toward lasting relief and better gut health.